| Highlights |
1. Post-intensive care syndrome (PICS) affects up to 80% of patients who survive the ICU. 2. Intensivists should attempt to minimize common modifiable risk factors for the development of PICS. These include higher cumulative doses of sedative drugs, immobility, delirium, sleep disturbances, and hyperglycemia. 3. The social and financial impact of PICS can be substantial; up to 50% of patients who survive ICU are dependent on family care support and up to 40% of previously working patients who survive ICU are unable to return to work one year after discharge. |
CLINICAL QUESTION A 56-year-old woman with a history of diabetes and obesity was admitted to the ICU for pneumonia. Her hospitalization was complicated by acute respiratory distress syndrome (ARDS), shock, acute renal failure, and central line-associated bacteremia. She required mechanical ventilation for 7 days, vasopressors for 5 days, and continuous renal replacement therapy for 4 days. She was noted to have severe delirium and agitation while she was intubated and required deep sedation on multiple occasions. She also demonstrated weakness and mobility problems and was discharged to a rehabilitation facility. She is currently in post-ICU follow-up 1 month after discharge. Her family reports problems with her memory. She scores 14/30 on the Montreal Cognitive Assessment, which corresponds to moderate cognitive impairment. Which of the following conditions is most associated with the development of long-term cognitive impairment? A: shock B: delirium C: acute renal failure D: bacteremia (See Response/Reasons at the end of the article) |
Post-intensive care syndrome ( PICS) has been recognized for more than 1 decade and is defined as a new or worsening deterioration in physical, psychological, or cognitive health, or a combination thereof, after a critical illness .
At hospital discharge, up to 80% of patients who survive the ICU will have symptoms of PICS
The objective of the present review is to describe the clinical manifestations of PICS and its impact on patients, families, and healthcare systems. The authors also discuss the relationship between PICS and the social determinants of health and outline a framework for evaluation and management.
| Clinical presentation of PICS |
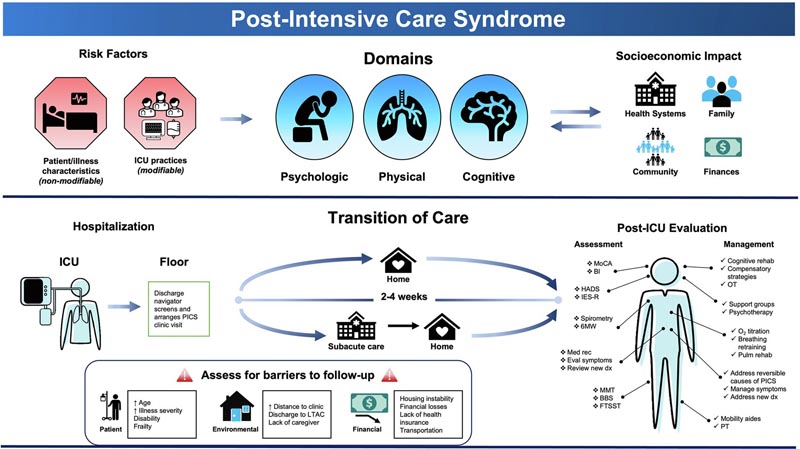
PICS may include impairments in cognition, mental health, physical function, or a combination of these following critical illness ( Figure 1A ).
> Cognitive domain
Survivors of critical illness are susceptible to cognitive dysfunction regardless of preexisting conditions, comorbidities, and age. Cognitive deficits can be both persistent , with one-third of patients surviving ICU presenting with deficits 1 year after hospitalization, or severe , reflecting the degree of impairment seen in moderate traumatic brain injury and dementia. Alzheimer’s.
Clinical manifestations may include declines in memory, executive function, mental processing speed, attention, or concentration, all of which together may prevent individuals from engaging in the type of purposeful, goal-directed behavior needed. to carry out activities of daily living and return to their premorbid functional state.
Among potentially modifiable risk factors , delirium has been the most studied. Even after adjusting for age, education, pre-existing cognitive function, disease severity, and exposure to sedative drugs, duration of delirium is an independent predictor of long-term cognitive decline ( Figure 1B ).
> Psychological domain
Psychiatric morbidity after critical illness is common. Anxiety, depression, and post-traumatic stress disorder (PTSD) are reported in 62%, 36%, and 39% of patients, respectively, with a high degree of symptom co-occurrence among these three conditions.
Patients who survive ICU are also at increased risk for suicidal and self-harm behaviors compared to hospital survivors who never required ICU admission.
Furthermore, sleep disorders are common after an ICU stay, occurring in up to 57% of patients 6 months after hospital discharge and are often associated with ongoing psychological deterioration.
Risk factors for psychological sequelae include younger age, previous mental health diagnoses, and need for mechanical ventilation. Pre-existing and in-hospital sleep disorders are associated with an increased risk of postmorbid sleep disorders ( Figure 1B ).
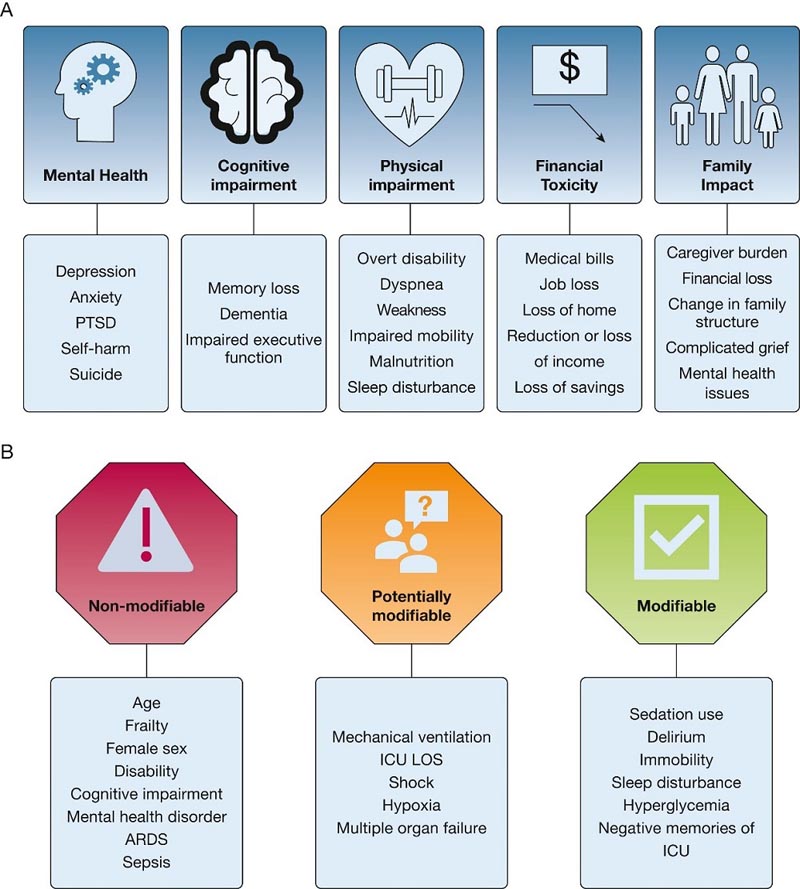
Figure 1 -Diagrams showing the clinical manifestations and risk factors of PICS (post-intensive care syndrome). A , Common sequelae of critical illness in patients surviving the ICU. B , Risk factors associated with PICS, categorized by degree of modifiability. LOS= length of stay; PICS=post-intensive care syndrome; PTSD=Post-traumatic stress disorder.
> Physical domain
Up to 80% of patients who survive the ICU experience new physical dysfunction at the time of discharge. The types of physical impairments vary and may include ICU-acquired weakness (ICU-AW), impaired lung function, and cachexia.
ICU-acquired weakness ( ICU-AW), defined as neuromuscular dysfunction without a plausible cause other than critical illness and its treatments, is often the result of critical illness myopathy, critical illness polyneuropathy Or a combination of both. This group of disorders is present in almost half of patients who survive the ICU and can manifest in a variety of ways, including poor mobility, weakness, contractures, and reduced exercise tolerance.
Among potentially modifiable risk factors, the uses of neuromuscular blockers and corticosteroids have historically been implicated in the development of critical illness myopathy, particularly when used in combination. However, the above data suggest that short-term use of these medications may be safe.
Additionally, patient mobilization (e.g., progressive mobilization starting with range of motion and eventually progressing to out-of-bed mobility activities) is a preventive measure known to reduce the risk of ICU-AW ( Figure 1B ). .
> Disability, health care use and mortality
The collective sequelae of critical illness can ultimately lead to frailty, disability, and reduced health-related quality of life (HRQoL). New or worsening frailty is seen in 40% of patients who survive the ICU 12 months after hospital discharge. Consequently, at least partial disability is detected in 20% of previously independent people one year after discharge with low scores predominantly attributed to reduced physical function.
Healthcare use patterns may also change after a critical illness, with an increased risk of rehospitalization that can last for years. More than half of patients are readmitted after hospital discharge, and in the year after critical illness, survivors show an increase in outpatient visits, emergency department visits, and hospitalizations compared to the previous year
Finally, the risk of death remains elevated even after patients have survived critical illness, with 1-year mortality rates as high as 21%. This risk is especially notable in patients who survive the ICU who received mechanical ventilation , whose one-year mortality can exceed 40%.
> Family and post intensive care syndrome (PICS)
The impact of surviving in the ICU can extend beyond the individual patient.
Between 25% and 50% of patients who survive the ICU require long-term family support that may resemble the burden of care seen in other chronic illnesses. In turn, caregivers may experience new psychological symptoms, collectively termed post-intensive care family syndrome . Prevalence is highly variable, ranging from 6% to 69% in the first 6 months and can last for years. The most common impairments include anxiety (73%), depression (50%), complicated grief (52%), and PTSD. (56%).
These symptoms generally decrease over time, but may persist in approximately one-third of people at 6 months, with associated low HRQoL and psychological distress reported for years thereafter. Risk factors for the development of family PICS can generally be classified into characteristics related to the patient, caregiver, and environment ( Figure 2 ).
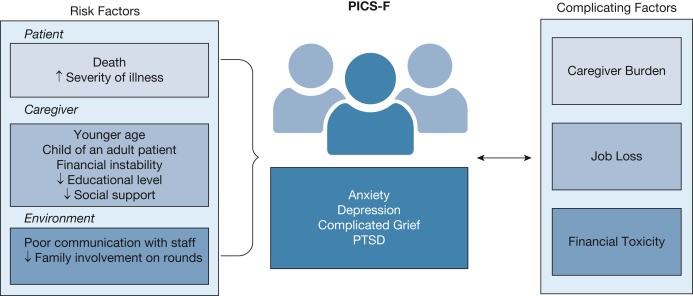
Figure 2 -Diagram showing the risk factors, clinical manifestations and complicating factors of the PICS family. PICS-F=post-intensive care-family syndrome; PTSD=Post-traumatic stress disorder .
> Financial toxicity
Patients who survive the ICU may experience significant financial toxicity . Less than half of previously employed ICU survivors return to work one year after a critical illness and about a third of patients remain unemployed after 5 years. Consequently, unemployment can lead to depleted savings, loss of health care coverage, and increased medical bills.
> Health equity
Health disparities and inequities exacerbate and are exacerbated by PICS. The dynamics that can influence incidence and recovery can be broadly classified into individual, community, health system, and policy-level factors ( Figure 3 ).
Age, sex, race, and income are some of the individual social determinants of health associated with long-term outcomes. Education is also an important factor, as a higher level of education is associated with higher odds of being free of PICS.
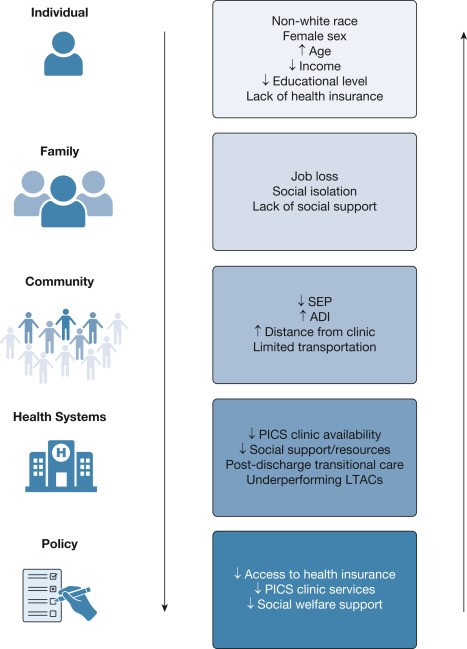
Figure 3 - Diagram showing socioeconomic factors exacerbated and exacerbated by post-intensive care syndrome. ADI= area deprivation index; LTAC=long-term acute care; PICS=post-intensive care syndrome; SEP=socioeconomic position.
From a health systems and policy perspective, restricted access to additional rehabilitation, ancillary services, and social resources propagates disparities that are known to inhibit successful recovery.
| PICS Clinic |
Multidisciplinary ICU recovery programs have been established to address the multifaceted long-term impairments observed in survivors of critical illness. Currently, there is substantial heterogeneity in clinic availability, structure, and staffing models.
Arranging the initial outpatient visit can be fraught with challenges because a large number of barriers to follow-up may exist ( Figure 4 ). Patient-level factors may include older age, greater severity of ICU illness, and disability. Financial and environmental barriers may involve lack of insurance, cost of transportation, and distance to the clinic. Additionally, many patients are transferred from the hospital to a rehabilitation facility before discharge, which may also decrease the likelihood of follow-up.
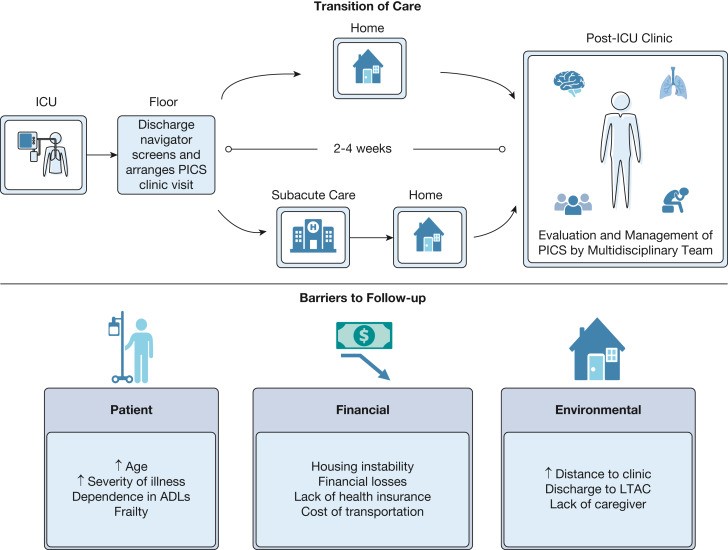
Figure 4 -Diagram showing the schedule of care and barriers to follow-up after critical illness. ADL=activity of daily living; LTAC= long-term acute care; PICS=Post intensive care syndrome.
| PICS Evaluation |
PICS assessment and management are evolving, and current recommendations are largely based on expert opinion and provider experience. Each PICS domain must be evaluated in a structured manner ( Figure 5 ), because otherwise more subtle degradations may be missed.
The initial evaluation should also include complete medication reconciliation, evaluation of new or persistent symptoms, detection of gaps in maintenance of medical care, and placement of any clinically indicated referral. Additionally, ICU admission as well as the expected course of recovery should be reviewed in detail with the patient.
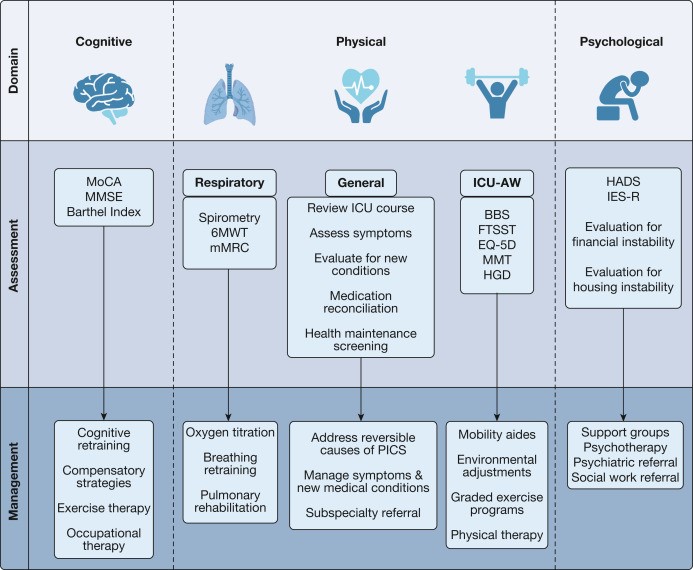
Figure 5 - Diagram showing evaluations by clinical provider. The specific clinician performing each evaluation may be modified based on local availability and experience. 6MWT=6 minute walk test; BBS=Berg Balance Scale; EQ-5D=EuroQol-5D; FTSST=five times standing test; HADS=Hospital Anxiety and Depression Scale; HGD=handgrip dynamometry; ICU-AW=ICU acquired weakness; IES-R=Impact Event Scale-Revised; mMRC=Modified Medical Research Council; MMSE=Mini-Mental State Examination; MMT=Manual muscle testing; MoCA=Montreal Cognitive Assessment; PICS=Post intensive care syndrome.
> Cognitive domain
Ideally, a battery of assessment types should be used to detect cognitive deficits, as they provide different information and can ensure that patients receive appropriate care.
Subjective cognitive symptoms, such as forgetfulness or increased dependence on caregivers, may indicate cognitive impairment.
The initial step in treating cognitive dysfunction should be to evaluate and manage any potentially reversible causes . These include, but are not limited to, medication side effects, sleep disorders, psychiatric conditions, and metabolic or nutritional disorders. After reversible causes are addressed, other treatment options may be considered.
> Psychological domain
Several post-ICU centers offer peer support groups through virtual or in-person platforms, which can have a number of benefits for patients. It is also important for clinicians to counsel patients on the expected recovery trajectory, normalizing their experience and validating their progress.
- Patients with persistent psychiatric deficits may benefit from referral to a mental health professional for appropriate treatment.
- Patients with depression may be treated with an antidepressant or psychotherapy alone, or in combination, which may be more effective.
> Physical domain
Methods for assessing ICU-acquired weakness (ICU-AW) are not widely accepted. Commonly used tools include manual muscle testing, manual dynamometry, the five-fold sit-to-stand test, and the Berg Balance Scale. The 6-minute walk test is recommended by the Society of Critical Care Medicine as a measure of lung and physical function. Bedside spirometry or complete lung function testing may also be helpful, particularly for ARDS survivors.
Because a variety of types of physical impairments can occur after a critical illness, other commonly encountered problems must also be addressed, such as newly diagnosed chronic conditions, sleep problems, and ICU-acquired injuries and devices.
| Future directions |
Although the COVID-19 pandemic brought much-needed attention to PICS, access to post-ICU care remains highly variable and the ideal model and optimal delivery of post-ICU care is unknown. Furthermore, the evidence base for interventions aimed at managing PICS, such as cognitive therapy and post-ICU support groups, is limited. To ensure that the needs of patients with PICS are met, future efforts should be directed toward studying the impact of existing interventions on patient outcomes, exploring new interventions with potential benefits, and determining the most effective structure of care delivery. after ICU.
Understanding PICS also represents an opportunity to improve care within the ICU, both in real time and in the future.
For clinicians , witnessing a patient’s recovery process can be educational and ultimately improve accuracy in predicting outcomes in the ICU and improve clinical decision making.
For ICU staff at centers without dedicated PICS clinics, education and appreciation of the impact of ICU interventions on non-mortality outcomes has the potential to improve ICU care by increasing surveillance on risk factors. modifiable risk of PICS, such as sedation and mobilization practices.
| Conclusions |
Survival in the ICU is often complicated by PICS, which causes physical, cognitive, and psychological impairments, as well as considerable morbidity. Its impact extends beyond individual patients to include families, healthcare systems, and society as a whole. Post-ICU clinics are an important tool for evaluating and managing PICS and may also represent a way to improve care within the ICU.
CLINICAL QUESTION A 56-year-old woman with a history of diabetes and obesity was admitted to the ICU for pneumonia. Her hospitalization was complicated by ARDS, shock, acute renal failure, and central line-associated bacteremia. She required mechanical ventilation for 7 days, vasopressors for 5 days, and continuous renal replacement therapy for 4 days. She was noted to have severe delirium and agitation while she was intubated and required deep sedation on multiple occasions. She also demonstrated weakness and mobility problems and was discharged to a rehabilitation facility. She is currently in post-ICU follow-up 1 month after discharge. Her family supports problems with her memory. She scores 14/30 on the Montreal Cognitive Assessment, which corresponds to moderate cognitive impairment. Which of the following conditions is most associated with the development of long-term cognitive impairment? A: shock B: delirium C: acute renal failure D: correct bacteremia: B: delirium Rationale : Delirium (choice B) is independently associated with long-term cognitive impairment even after adjusting for age, education, sedation, disease severity, and pre-existing cognitive function. Furthermore, longer duration of delirium is associated with decreased global cognition and executive function at 1 year in critical illness survivors. Strategies such as adoption of the ABCDEF bundle, which includes assessment for delirium, daily testing for spontaneous awakening and breathing, avoidance of inappropriate or excessive sedation, early mobilization, and presence of family, may reduce the incidence of delirium and the risk of subsequent cognitive impairment and should be used. as a preventative measure for PICS, which is seen in up to 80% of patients who survive the ICU. Although shock (choice A) can also be a risk factor for long-term cognitive impairment, it is less frequently associated with this complication than delirium. Acute renal failure (choice C) and bacteremia (choice D) are not known to be associated with long-term cognitive dysfunction. |
















