There is already strong evidence that people living with cardiovascular disease are disproportionately affected by poor air quality and extreme temperatures , largely due to climate change, the biggest threat to human health of the 21st century. In a special themed issue of the Canadian Journal of Cardiology , leading experts comprehensively review how climate change is occurring and increasing the risk of cardiovascular disease and provide practical advice on how to become a climate-smart cardiovascular healthcare provider.
Not long ago, climate change was a fringe issue, considered to only affect rare species and ignored by many. The 2019 Global Burden of Diseases, Injuries and Risk Factors (GBD) Study estimated that nine million people died prematurely due to air pollution in 2019. Nearly 62% of these deaths were related to cardiovascular diseases, which which highlights the fact that climate change is not only a general health issue, but also a major cardiovascular health issue.
Minimize long-term exposure to pollutants to prevent cardiovascular disease
The guest editors explain: “The health effects of extreme heat and poor air quality gained notable attention recently due to the 2021 heat dome that caused 619 heat-related deaths in British Columbia, Canada, the European summer of 2022 which was the hottest in the world and caused approximately 61,672 heat-related deaths, and the wildfires in Quebec, Canada, which caused poor air quality in vast areas of northeastern America during the summer of 2023. In this context, It has never been more relevant to understand how it affects the environment. In addition to extreme weather and air pollution being associated with cardiovascular events, it is increasingly recognized that the comprehensive exposure of individuals and populations to the environment around them (the exposome ) throughout life is closely related to health and cardiovascular well-being.
Issam Motairek, MD, Case Western Reserve University School of Medicine, and colleagues review the relationship between the exposome and cardiovascular health, highlighting epidemiological and mechanistic evidence of environmental exposures on cardiovascular disease. This review also reinforces the importance of minimizing long-term exposure to pollutants for the prevention of cardiovascular disease.
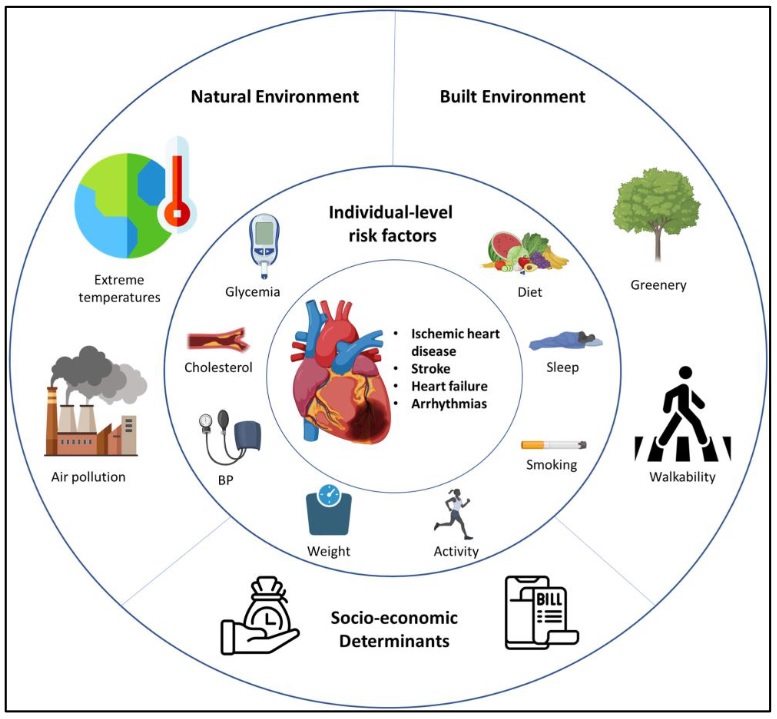
Figure : Exposome characteristics associated with cardiovascular health (Credit Canadian Journal of Cardiology, created with BioRender.com).
Airborne nanoaggressors ( air pollution), dietary nanoaggressors (hyper-processed foods), the level of greening, and an environment that encourages (or does not) physical activity are the main environmental determinants of heart health. François Reeves, MD, FRCPC and Brian J. Potter, MDCM, SM, FRCPC, both from the University of Montreal, propose a cardioenvironmental model for cardiovascular risk assessment of easily assessable factors by asking:
(1) who is my patient? (family history, ethnicity, traditional risk factors, body mass index and comorbidities).
(2) what does my patient do? (eating habits, smoking, drugs, physical activity).
(3) where does my patient live? (air quality, food quality, urban environment).
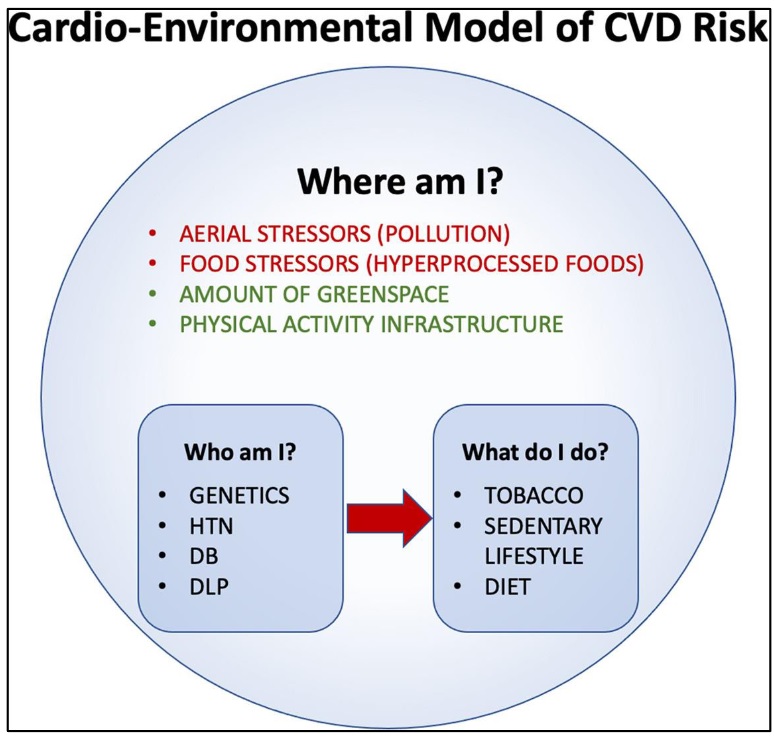
Figure : Cardioenvironmental model of cardiovascular disease risk . The authors illustrate how air pollution, hyper-processed foods, the amount of green space, and population activity levels are now considered the four main environmental determinants of cardiovascular health and provide a framework for how these considerations could be incorporated into the clinical risk assessment (Credit Canadian Journal of Cardiology).
Climate change and air pollution make each other worse
A review by Barrak Alahmad, MD, PhD, Harvard TH Chan School of Public Health, and colleagues shows that climate change and air pollution worsen each other , leading to several ecosystem-mediated impacts. They highlight how the increase in warm climates as a result of climate change has increased the risk of major air pollution events, such as severe wildfires and dust storms, and that altered atmospheric chemistry and changing patterns of weather conditions can promote the formation and accumulation of air pollutants, a phenomenon known as climate penalty . Extreme heat events, in which temperature and/or humidity are high enough to generate health impacts at the population level, are an important consequence of the acceleration of the climate crisis.
Daniel Gagnon, PhD, and colleagues describe how the human body interacts with a hot environment during physical activity, summarize current guidelines for physical activity in hot climates, and conclude with practical strategies to encourage safe physical activity in hot climates. David Kaiser MD, MSc, McGill University and colleagues note that cardiovascular physicians and researchers are uniquely positioned to help prevent heat wave mortality by identifying patients who are most at risk and using education, referrals and promotion to contribute to public health interventions. High blood pressure is responsible for almost nine million deaths annually worldwide; Environmental pollution increases the incidence of hypertension and exacerbates its severity.
Poor air quality increases the risk of many cardiovascular diseases
Environmental offenders include the adverse vascular effects of air pollution, lack of green space, increased risk of infection, lack of physical activity, temperature effects, noise pollution, circadian rhythm disruption, and disparities. economic conditions, such as limited access to medical care. Francisco J. Ríos, PhD, McGill University Health Center, and his colleagues highlight their crucial impact and how these determinants influence diverse communities. They also address opportunities and challenges for new research to address knowledge gaps in our understanding of the molecular mechanisms through which environmental factors influence the development of hypertension and associated cardiovascular diseases.
Poor air quality increases the risk of many cardiovascular diseases, including atherosclerosis and, as a result, the incidence of myocardial infarction, stroke and cardiovascular death. Additionally, acute and chronic increases in air pollution increase the risk of atrial and ventricular arrhythmias, the incidence of heart failure, and heart failure-related hospitalizations. A review by Matthew Bennett, MD, and his colleagues examines the association between acute and chronic exposure to air pollution and the incidence, morbidity and mortality of arrhythmias, and the putative pathophysiological mechanisms. They highlight several pathways that mediate this association, including increases in inflammation, oxidative stress, mitochondrial and autonomic dysfunction, cardiac structural changes, and altered function of calcium, potassium, and sodium channels .
Cavin K. Ward-Caviness, PhD, and Wayne E. Cascio, MD, both of the U.S. Environmental Protection Agency, found substantial evidence linking exposure to air pollution with the incidence of heart failure and related hospitalizations. They propose that more studies specifically to identify data gaps will greatly improve our knowledge about the susceptibility of people with heart failure and interventions to reduce risks.
The World Health Organization has reported that more than 1.6 million years of healthy life are lost each year due to traffic-related noise in Western Europe. Thomas Münzel, MD, University Medical Center Mainz, and his colleagues provide an overview of the effects of noise on non-auditory cardiovascular health, including acute and chronic ischemic heart disease, heart failure, arrhythmia, and stroke . They also provide evidence from translational studies of human and experimental noise and discuss maneuvers to effectively mitigate noise.
Khalid Al-Thalji, MD, University of Toronto, and colleagues describe how to incorporate environmental cardiology into medical education to create climate-smart cardiovascular health care providers to minimize the cardiovascular effects of climate change on patients and the general population, improve awareness of these effects and create climate change advocates within the cardiovascular community. The guest editors comment: “By educating cardiovascular health professionals, students, the public, and policymakers about how and to what extent climate change increases the risk of cardiovascular disease, we can minimize the impact of environmental factors on cardiovascular health.
Aditya Khetan, MD, McMaster University, and Sadeer Al-Kindi, MD, Case Western Reserve University, explain how patients can adapt to environmental risk and, in particular, what recommendations should be given to high-risk patients during the days of "bad air" and during times of hot or cold temperatures. The guest editors conclude: “The association between climate change and cardiovascular events is clear. Cardiovascular health professionals, as healthcare leaders and educators, can play a leadership role in minimizing the effect of environmental factors on cardiovascular health. “Ongoing and future research will help manage the influence of environmental factors on cardiovascular health to thrive on a warmer planet.”
















