Key points What are the utilization rates and comparative safety outcomes of robotic-assisted cholecystectomy versus laparoscopic cholecystectomy in the United States? Findings This cohort study of claims data for Medicare beneficiaries identified 1,026,088 who underwent cholecystectomy between 2010 and 2019. Robot-assisted cholecystectomy rates increased 37-fold and this procedure was associated with a higher rate of bile duct injury compared with laparoscopic cholecystectomy. (0.7% vs. 0.2%). Meaning In the absence of other advantages over a procedure that is already minimally invasive, the findings of this study call into question the role of the robotic platform for cholecystectomy. |
The United States is a global outlier in the adoption of robotic-assisted surgery. While the technology was initially marketed for its ability to overcome technical challenges associated with certain procedures (e.g., prostatectomy), it has since expanded into domains with weaker clinical justification and limited evidence. Recent studies suggesting inferior oncologic outcomes after robotic-assisted surgery for breast cancer 5 and cervical cancer led the US Food and Drug Administration to issue a public safety warning.
Evidence in general surgery, the field currently experiencing the most rapid adoption of robotic-assisted procedures, suggests that these patterns may expose patients to harm as surgeons learn the new surgical approach. For example, while cholecystectomy remains one of the most routine operations performed by general surgeons, a recent multifold increase in the use of robotic-assisted surgical procedures has fueled ongoing debate about the potential safety implications of this. change in practice.
Importance
Robotic-assisted cholecystectomy is being rapidly adopted into practice, in part due to the belief that it offers specific technical and safety advantages over traditional laparoscopic surgery. It is still unclear whether robot-assisted cholecystectomy is safer than laparoscopic cholecystectomy.
Aim
To determine the acceptance of robotic-assisted cholecystectomy and analyze its comparative safety compared to laparoscopic cholecystectomy.
Design, environment and participants
This retrospective cohort study used Medicare administrative claims data for non-federal acute care hospitals from January 1, 2010 to December 31, 2019.
Participants included 1,026,088 fee-for-service Medicare beneficiaries aged 66 to 99 years who underwent cholecystectomy with continuous Medicare coverage for 3 months before and 12 months after surgery. Data was analyzed from August 17, 2022 to June 1, 2023.
Exposure
Surgical technique used to perform cholecystectomy: robotic versus laparoscopic approach.
Main results and measures
The primary outcome was the rate of bile duct injury requiring definitive surgical reconstruction within 1 year after cholecystectomy.
Secondary outcomes were the composite outcome of bile duct injury requiring less invasive postoperative endoscopic or surgical biliary interventions and the overall incidence of 30-day complications.
A multivariable logistic analysis was performed adjusting for patient factors and grouping within hospital referral regions. An instrumental variable analysis was performed, taking advantage of regional variation in the adoption of robotic-assisted cholecystectomy within hospital referral regions over time, to account for potential confounding factors arising from unmeasured differences between groups. of treatment.
Results
A total of 1,026,088 patients (mean [SD] age, 72 [12.0] years; 53.3% women) were included in the study. The use of robotic-assisted cholecystectomy increased 37-fold, from 211 of 147,341 patients (0.1%) in 2010 to 6,507 of 125,211 patients (5.2%) in 2019.
Compared with laparoscopic cholecystectomy, robotic-assisted cholecystectomy was associated with a higher rate of bile duct injury requiring definitive surgical repair within 1 year (0.7% vs 0.2%; relative risk [RR] , 3.16 [95% CI, 2.57-3.75]).
Robotic-assisted cholecystectomy was also associated with a higher rate of postoperative biliary interventions, such as endoscopic stenting (7.4% vs. 6.0%; RR, 1.25 [95% CI, 1.16 -1.33]).
There were no significant differences in overall 30-day complication rates between the 2 procedures. Instrumental variable analysis, which was designed to account for possible unmeasured differences in the treatment groups, also showed that robotic-assisted cholecystectomy was associated with a higher rate of bile duct injury (0.4% vs. 0.2%; RR, 1.88 [95% CI, 1.14-2.63]).
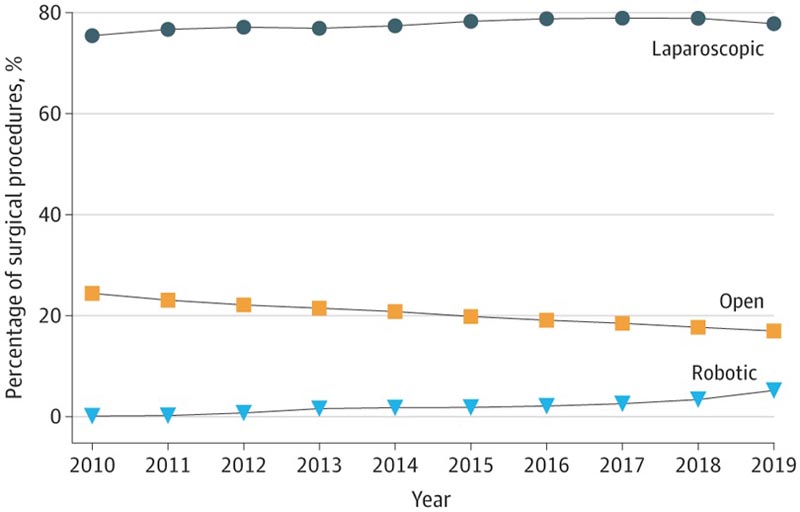
Figure : The number of patients included each year was 147,341 for 2010; 140,100 for 2011; 136,185 for 2012; 131,329 for 2013; 127 36 for 2014; 129,614 for 2015; 129,367 for 2016; 126,494 for 2017; 124,738 for 2018; and 125,211 for 2019.
Conclusions and relevance This cohort study’s finding of significantly higher rates of bile duct injury with robotic-assisted cholecystectomy compared with laparoscopic cholecystectomy suggests that the utility of robotic-assisted cholecystectomy should be reconsidered , given the existence of an laparoscopic procedure that is already minimally invasive and predictably safe. |
















