Nonalcoholic fatty liver disease ( NAFLD) has become the most common cause of chronic liver disease, affecting approximately 80 million people in the United States. The rapid rise of end-stage liver disease and NAFLD-related hepatocellular carcinoma and its severe phenotype, non-alcoholic steatohepatitis, has resulted in considerable economic burden and stress on healthcare systems worldwide.
Cardiovascular diseases (CVD) and malignancies have been identified as the most common causes of death in NAFLD. Therefore, identifying modifiable lifestyle factors for NAFLD and its main causes of mortality could potentially reduce its population burden.
Physical activity ( PA) and diet quality (DQ) are modifiable risk factors that have been shown to be strongly associated with NAFLD and its severity.
Observational and interventional studies have reported that increased PA, including different modalities, and better DQ are associated with a lower risk of nonalcoholic fatty liver disease (NAFLD), nonalcoholic steatohepatitis, and advanced fibrosis.
In several large prospective cohort studies, moderate-to-vigorous intensity PA (MVPA) and higher DQ as assessed by the Healthy Eating Index (HEI), the Alternative Healthy Eating Index (AHEI), and the Dietary approaches to stop hypertension have been associated with lower chronic disease risk scores and all-cause mortality, related to cardiovascular disease and cancer.
Methods
Using data from the 2011-2014 National Health and Nutrition Examination Survey, 3548 participants with a fatty liver index ≥60 were included. BP was collected using a triaxial wrist accelerometer and expressed as 2 metrics using monitor-independent motion summary (MIMS) units: the average daily MIMS, which represents volume, and the 30-minute peak MIMS, which is the average of the highest. 30 MIMS min/d and represents the intensity.
Diet quality ( DQ) was evaluated by the Healthy Eating Index-2015. Mortality monitoring was recorded by linking the National Death Index until December 31, 2019.
Results
Our analyzes revealed a dose-dependent nonlinear association of PA (volume and intensity) with all-cause mortality and a dose-dependent linear association of DQ with all-cause mortality.
The maximum protective dose of PA volume was observed at 14,300 MIMS/min (adjusted HR: 0.20, 95% CI: 0.11–0.38). The maximum protective dose of PA intensity was observed at 54.25 MIMS/min (adjusted HR: 0.10, 95% CI: 0.05–0.23), beyond which mortality risks stabilized .
The 2015 Healthy Eating Index showed its maximum protective effect at 66.17 (adjusted HR: 0.54, 95% CI: 0.40–0.74).
Higher levels of PA (volume and intensity) were associated with a lower risk of cardiovascular disease-related mortality, but not cancer. A healthier diet was associated with a reduced risk of cardiovascular mortality and cancer.
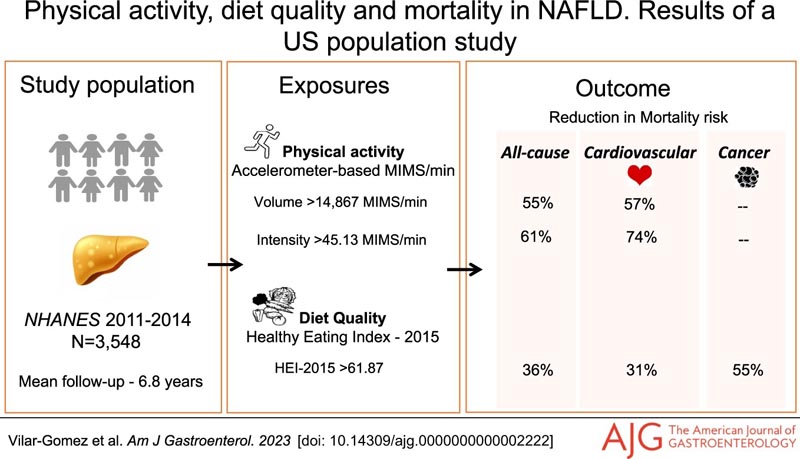
Conclusion In conclusion, among US adults with NAFLD, greater adherence to healthier eating patterns and greater total volume and intensity of PA were associated with lower risk of all-cause and CVD mortality. Following healthier eating patterns also conferred protection against cancer-related mortality. The survival benefits achieved with higher levels of DQ and PA were also observed in participants without NAFLD. In particular, the current study will help guide our understanding of MIMS BP/min metric thresholds aligned with survival rates using free-living wrist accelerometry data from a nationally representative sample (NHANES). |
Final message
Our findings suggest that higher cumulative daily physical activity effort and diet quality are associated with lower cardiovascular and all-cause mortality in US adults with nonalcoholic fatty liver disease (NAFLD).
















