Persistent disability and risks of death were associated with inflammatory levels in patients after major abdominal surgery.
Summary Postoperative systemic inflammation is strongly associated with surgical outcomes, but its relationship with patient-centered outcomes is largely unknown. Detection of excessive inflammation and surgical and patient factors associated with patient-centered adverse outcomes should inform preventive treatment options that will be evaluated in clinical trials and current clinical care. This retrospective cohort study analyzed prospectively collected data from 3000 high-risk elective major abdominal surgery patients in the Restrictive Versus Liberal Fluid Therapy for Major Abdominal Surgery (RELIEF) trial from 47 centers in seven countries from May 2013 to September 2013. 2016. Co-primary endpoints were persistent disability or death up to 90 days after surgery, and quality of recovery using a 15-item quality of recovery score at days 3 and 30. Secondary endpoints included : all-cause mortality at 90 days and 1 year; septic complications; acute kidney injury; unplanned admission to intensive care unit/high dependency unit; and total hospital and intensive care unit stays. Patients were assigned to quartiles of maximum postoperative C-reactive protein concentration through day 3, after multiple imputations of missing values. The lowest (reference) group, quartile 1, C-reactive protein ≤ 85 mg.l-1, was compared with three inflammation groups: quartile 2 > 85 mg.l-1 to 140 mg.l-1; quartile 3 > 140 mg.l-1 to 200 mg.l-1; and quartile 4 > 200 mg.l-1 to 587 mg.l-1. Greater postoperative systemic inflammation had a higher adjusted hazard ratio (95% CI) of persistent disability or death up to 90 days after surgery, quartile 4 versus quartile 1 was 1.76 (1.31–2.36 ), p < 0.001. Increasing inflammation was associated with an increasing decrease in the estimated risk-adjusted medians (95% CI) for quality of recovery, with the difference from quartile 4 to quartile 1 being -14.4 (-17. 38 to -10.71), p < 0.001 on day 3, and - 5.94 (-8.92 to -2.95), p < 0.001 on day 30. Marked postoperative systemic inflammation was associated with an increased risk of complications, poor quality of recovery, and persistent disability or death up to 90 days after surgery. |
Complications following major surgery contribute to approximately eight million deaths annually. The impact of perioperative inflammation and immune function on surgical outcomes is appreciated now more than ever following the global surgical collaboration’s findings on the timing of surgery after SARS-CoV-2 infection. Inflammation after major abdominal surgery is essential and is balanced by pro- and anti-inflammatory processes within the innate and adaptive immune systems, stimulating natural repair and healing.
However, dysregulated hyperinflammation and/or immunosuppression may increase the risk of postoperative complications and organ dysfunction and contribute to poorer quality of recovery, persistent disability, or death. Most analyzes to date use plasma C-reactive protein (CRP) concentrations to assess the impact of different levels of inflammation on short-term surgical and infectious complications and long-term overall survival. The consequences of higher levels of postoperative systemic inflammation on patient-centered outcomes are unclear.
Accordingly, we investigated the relationship between postoperative systemic inflammation and the quality of recovery, disability, and complications after major abdominal surgery. Our primary hypothesis was that adults with higher levels of postoperative systemic inflammation had a higher complication rate, poorer quality of recovery, and poor disability-free survival after major abdominal surgery compared to patients with lower levels. of postoperative systemic inflammation.
Comments
In a study published in Anesthesia , researchers found significant correlations between postoperative systemic inflammation and worse outcomes in patients recovering from major abdominal surgery.
Postoperative complications after major surgeries cause millions of deaths each year. Immunosuppression and/or hyperinflammation are suspected to contribute to these outcomes, which may increase a person’s vulnerability to organ dysfunction, persistent disability, worsening recovery from surgery, and even death. Much of this research reaches these conclusions by monitoring plasma levels of C-reactive protein (CRP); However, as the authors note, the influence of postoperative systemic inflammation on patient outcomes remains inconclusive. To address this gap in the literature, researchers conducted a retrospective cohort study to explore associations between inflammation and various outcomes after major abdominal surgery.
Data were collected from the RELIEF (restrictive versus liberal fluid therapy for major abdominal surgery) trial (a multicenter study evaluating different intravenous fluid regimens administered to patients) from May 2013 to September 2016. Patients with varying levels of systemic inflammation , measured with PCR: were analyzed in 47 centers in 7 countries.
The co-primary endpoints for this study were persistent disability or death within 90 days after surgery, as well as a 15-item score of an assessment of the quality of recovery on days 3 and 30. Secondary outcomes were all-cause mortality at 90 days and 1 year, acute kidney injury, septic complications, unplanned admission to intensive care unit/high dependency unit (ICU/HDU), total length of hospitalization; and re-admission to the hospital. The researchers divided the data into quartiles based on the increase in peak CRP concentration at 3 days postoperatively. The lowest quartile was known as “reference group” (Q1) and the others were considered “inflammation groups” (Q2-Q4).
In total, 2,533 patients were eligible for analysis, having received at least one CRP measurement up to the third postoperative day. The reference group included 639 people with maximum levels up to day 3 < 85 mg/L –1, which “reflects a resolving host response, which promotes wound healing and tissue repair.” The highest quartile (Q4) was composed of 618 individuals who recorded a maximum CRP until day 3 of 587 mg/L –1.
Up to day 90 after surgery, an increasing proportion of patients affected by persistent disability or who died was observed in all inflammation groups compared to the reference (10.8% [Q1] vs. 13.2% [Q2 ] vs. 18.2% [Q3] vs. 25.6% [P4]). For patients who had a day 3 peak CRP greater than 200 mg/L –1, and for each subsequent increase of 100 mg/L –1, the researchers found they had significantly increased risks for these outcomes (P < 0.001). .
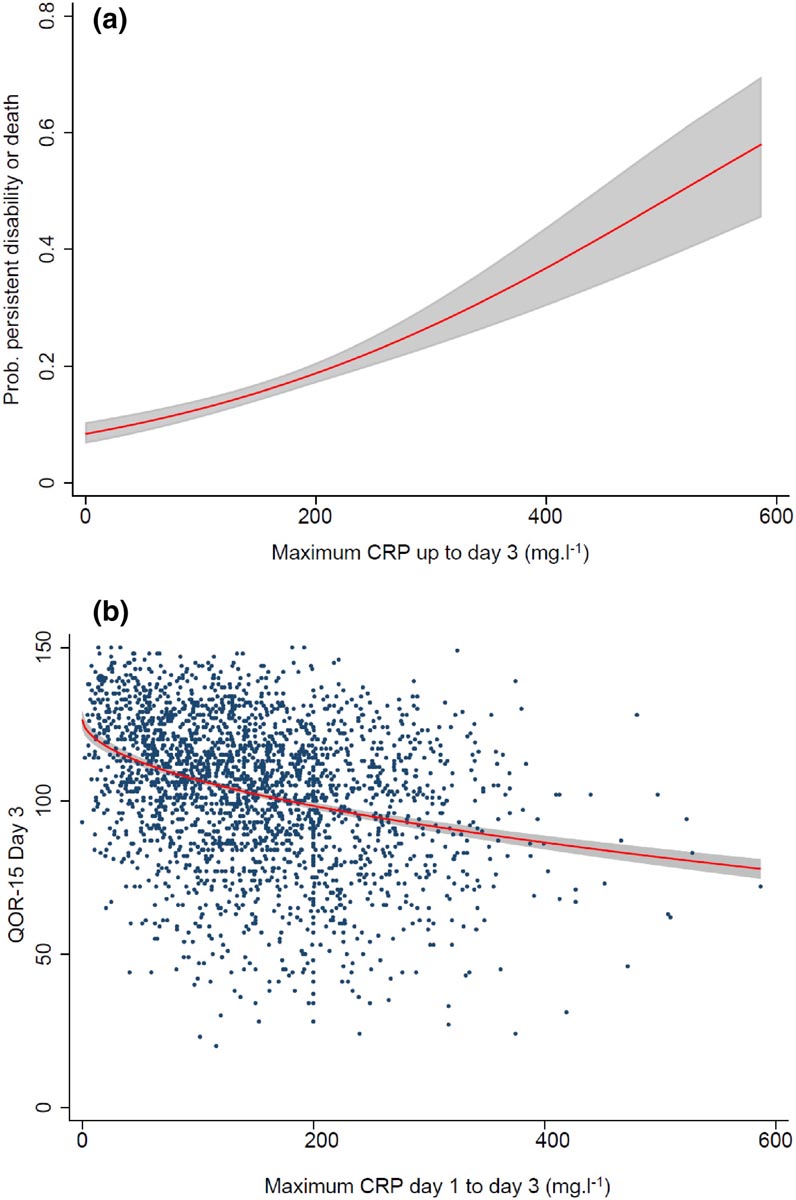
Figure : (a) The relationship between the maximum measured postoperative C-reactive protein (CRP) concentration (mg.l-1) up to day 3 and the probability of persistent disability or death up to day 90 after major abdominal surgery; (b) the relationship between the maximum CRP concentration on the postoperative day (mg.l-1) until day 3 and the quality of recovery on day 3. Shaded bands are 95% CI.
Correlative evidence between inflammatory states and patient outcomes supports the use of peak postoperative CRP as a valuable inflammatory marker
Reports of the quality of patient recovery also increasingly declined in the upper quartiles; the authors note that even minimal differences in postoperative inflammation correlate with significantly reduced recovery at day 3. Similarly, patient risks for acute kidney injury, septic complications, unplanned ICU/UHD admission, hospital stays longer durations and unexpected hospital readmissions grew with increasing inflammation ( p < 0.001 for each endpoint). However, at day 90 and at one year, no significant differences were observed between the groups.
Overall, the authors note that the correlative evidence between inflammatory states and patient outcomes supports the use of peak postoperative CRP (up to day 3) as a valuable inflammatory marker. Their findings reinforce the idea that CRP should be monitored in patients who have undergone surgical procedures to guide discharge decisions and as an assessment tool to predict recovery risks.
Discussion
We have demonstrated a significant association between higher levels of postoperative systemic inflammation, as measured by maximum postoperative CRP up to day 3, with severe complications, poorer quality of recovery, and persistent disability or death up to 90 days after major abdominal surgery.
The postoperative stress response includes neurohumoral and inflammatory-immune components that are determined by the magnitude of the surgical injury, modified by age, coexisting medical conditions, and anesthesia (immune modulation). Postoperative CRP concentrations reflect the level of cytokine (eg, interleukin-6) and chemokine release in response to tissue injury. C-reactive protein levels have been shown to reliably reflect the magnitude of the surgical injury and are lower after minimally invasive/laparoscopic surgery. Numerous systematic reviews of retrospective analyzes in colorectal surgery have highlighted that day 3 postoperative CRP > 150 mg.l-1 is associated with infectious complications and worse overall survival.
This analysis is the largest international multicenter observational study to date describing the association between postoperative systemic inflammation, as measured by CRP, and patient-centered outcomes after major abdominal surgery. However, high postoperative CRP levels on day 3 are significantly associated with adverse postoperative outcomes, and postoperative CRP > 200 mg.L was associated with a higher risk of serious complications, poorer quality of recovery, and persistent disability or death up to 90 days after surgery. Prediction, early detection, and targeted treatment strategies based on early CRP measurement may be an important step toward better monitoring and treatment of patients.
















