Canadian Society of Cardiology Classification of Acute Atherothrombotic Myocardial Infarction According to Stages of Severity of Tissue Injury: An Expert Consensus Statement
Summary
Myocardial infarction (MI) remains a leading cause of morbidity and mortality. In atherothrombotic MI (ST-elevation MI and type 1 non-ST-elevation MI), occlusion of the coronary artery causes ischemia. Subsequent cardiomyocyte necrosis evolves over time as a wave front within the territory at risk. The spectrum of ischemia-reperfusion injury is broad: it may be minimal in aborted MI or myocardial necrosis may be extensive and complicated by microvascular obstruction and reperfusion hemorrhage. Established risk scores and infarction classifications help with patient management, but do not consider the characteristics of the tissue injury. This document describes the Canadian Society of Cardiology classification of acute myocardial infarction. It is an expert consensus formed on the basis of decades of data on atherothrombotic MI with reperfusion therapy.
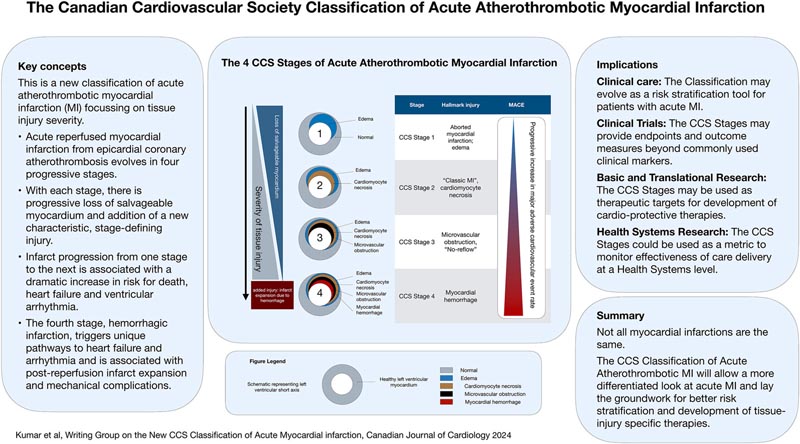
Four stages of progressive deterioration of myocardial tissue injury are identified: (1) aborted MI (minimal or no myocardial necrosis); (2) MI with significant cardiomyocyte necrosis but no microvascular injury; (3) cardiomyocyte necrosis and microvascular dysfunction leading to microvascular obstruction (i.e., “non-reflow”); and (4) microvascular and cardiomyocyte necrosis leading to reperfusion hemorrhage.
Each stage reflects the progression of tissue pathology from myocardial ischemia and reperfusion injury from the previous stage. Clinical studies have demonstrated worse remodeling and increased adverse clinical outcomes with progressive injury. In particular, microvascular injury is of particular importance, and the most severe form (hemorrhagic MI) leads to infarct expansion and risk of mechanical complications. This classification has the potential to stratify risk in patients with MI and lay the foundation for the development of new therapies for MI, specific to the stage of injury and based on tissue pathology.
Comments
Canadian Cardiovascular Society consensus statement published in the Canadian Journal of Cardiology paves the way to refine treatment and provide individualized care
First four-stage classification of heart attack based on heart muscle damage published
Heart attacks or acute myocardial infarction (MI) are one of the leading causes of death worldwide. The recently published Canadian Cardiovascular Society Classification of Acute Myocardial Infarction (CCS-AMI) appearing in the Canadian Journal of Cardiology presents a four-stage classification of heart attack based on heart muscle damage. This work by a group of leading experts has the potential to more accurately stratify risk in heart attack patients and lays the foundation for the development of new therapies based on tissue pathology and specific to the stage of injury.
Lead author Andreas Kumar, MD, MSc, Northern Ontario School of Medicine University and Department of Cardiovascular Sciences, Health Sciences North, Sudbury, ON, Canada, explains: “MI remains a leading cause of morbidity and mortality. Existing tools classify MIs using the patient’s clinical presentation and/or the cause of the heart attack, as well as ECG findings. Although these tools are very useful in guiding treatment, they do not consider the details of the underlying tissue damage caused by the heart attack. This expert consensus, based on decades of data, is the first classification system of its kind ever published in Canada and internationally. It offers a more differentiated definition of heart attacks and improves our understanding of acute atherothrombotic MI. At the tissue level, not all heart attacks are the same; “The new CCS-AMI classification paves the way for the development of more refined therapies for MI, which could ultimately result in improved clinical patient care and improved survival rates.”
The CCS-AMI classification describes damage to the heart muscle after MI in four sequential, progressively severe stages. Each stage reflects the progression of tissue pathology from myocardial ischemia and reperfusion injury from the previous stage. It is based on strong evidence about the effect an MI has on the heart muscle.
As damage to the heart increases through each progressive stage of CCS-AMI, patients are at dramatically increased risk of complications such as arrhythmia, heart failure, and death. Appropriate therapy can potentially halt the progression of the injury and stop the damage at an earlier stage.
Stage 1: Aborted MI (minimal or no myocardial necrosis). Minimal or no damage to the heart muscle. In the best case, the entire area of myocardium at risk can be saved. Stage 2 : MI with significant cardiomyocyte necrosis, but without microvascular injury. Damage to the heart muscle and no injury to the small blood vessels of the heart. Revascularization therapy will result in restoration of normal coronary flow. Stage 3 : MI with cardiomyocyte necrosis and microvascular dysfunction leading to microvascular obstruction (i.e., “no reflux”). Damage to the heart muscle and blockage of small blood vessels in the heart. The rate of major adverse cardiac events increases 2- to 4-fold in long-term follow-up. Stage 4 : MI with cardiomyocytes and microvascular necrosis leading to reperfusion hemorrhage. Damage to the heart muscle, blockage and rupture of small blood vessels causing bleeding in the heart muscle. This is a more severe form of microvascular injury and the most severe form of ischemia-reperfusion injury. It is associated with a further 2- to 6-fold increase in the rate of adverse cardiac events in long-term follow-up. |

Figure : Schematic representation of the 4 stages of the Canadian Cardiology Society (CCS) classification of acute atherothrombotic myocardial infarction in a macroscopic heart. CCS stage 1: aborted myocardial infarction (MI) with myocardial edema and minimal or no cardiomyocyte necrosis. CCS stage 2: MI with cardiomyocyte necrosis, but without microvascular injury. CCS stage 3: MI with microvascular obstruction. CCS stage 4: MI with reperfusion hemorrhage. Although rare extracapillary erythrocytes can be seen in stage 3, there is massive extravasation and macroscopic myocardial hemorrhage that defines stage 4.
Dr. Kumar concludes: The new classification will help differentiate heart attacks based on the stage of tissue damage and allow healthcare providers to more accurately estimate a patient’s risk of arrhythmia, heart failure and death. “It is hoped that CCS-AMI will ultimately lead to better care, better recovery and improved survival rates for heart attack patients.”
In an accompanying editorial, Prakriti Gaba, MD, Brigham and Women’s Hospital, Harvard Medical School, and Deepak L. Bhatt, MD, MPH, Mount Sinai Heart, Icahn School of Medicine at Mount Sinai, comment: “Kumar et al. They present a novel and intriguing four-level classification scheme of patients with acute myocardial infarction. This allows the unique utilization of prognostic pathologic features to help distinguish between high- and low-risk acute MI patients. Greater access to cardiovascular MRI would be needed to implement this new clinical approach widely; however, for research on emerging diagnostic and therapeutic strategies, it could be implemented immediately.”
Implications for clinical care and research.
We envision this classification to be an important framework for advancing clinical care and research. Clinical translation could help with risk stratification of patients; The risk of cardiovascular complications increases with each stage, from a comparatively low risk in CCS stage 1 (aborted MI) to the highest risk of adverse events in stage 4, including the risk of infarct expansion and mechanical complications. Application of the classification we have presented here can improve clinical care by differentiating high- and low-risk patients . Improving our understanding of the progression of injury stages could lay the foundation for the development of much-needed cardioprotective therapies.
There is a tremendous amount of research on ventricular remodeling, heart failure, and arrhythmia after acute myocardial infarction. Most studies take into account the underlying clinical characteristics of the patient (such as STEMI vs. NSTEMI, LV ejection fraction), but do not take into account the underlying tissue changes associated with MI. There are compelling data supporting that ventricular remodeling and arrhythmia risk are highly dependent on the composition of the underlying tissue . The classification presented here has the potential to allow assessment of heart failure and arrhythmia risk in the context of stages of tissue injury severity. This could lead to a more refined understanding of the pathophysiology, arrhythmia, and risk of heart failure after myocardial infarction and could profoundly affect patient treatment in the future.
The new classification could allow research and development of more differentiated and specific therapies for the stage of tissue injury; It seems plausible to assume that optimal medical therapies for acute MI will evolve to be different at each stage, because the underlying tissue injury is very different at each stage. Therefore, future clinical trials could benefit from applying the CCS classification of acute MI for subgroup analyses.
Myocardial ischemia and reperfusion injury are progressive; Cardioprotective therapeutic interventions could aim to stop the progression of tissue injury to the next worse stage. The classification presented here provides a metric to capture and document the extent of tissue injury in clinical trials. The CCS stages of acute MI could be applied as outcome measures and endpoints for research in patients with acute MI. Incorporating tissue injury endpoints into clinical research could help identify therapeutic opportunities that would otherwise go unrecognized if only clinical endpoints and traditional outcome measures were used. The CCS stages of acute MI could serve as therapeutic targets in this context.
Triage stages could also be applied as quality outcome measures to evaluate the effectiveness of healthcare systems, beyond traditional measures such as door-to-balloon time.
In a patient presenting with an acute MI, the ultimate goal would be to limit tissue injury to stage 1, where the patient remains at low risk and the injury is minimal and largely or completely reversible.
In summary, future personalized therapies and research in acute myocardial infarction should take into account the type and severity of tissue injury; The CCS classification of acute MI presented in this document is a tool to facilitate this.
Panorama
The CCS classification of acute MI developed by expert consensus captures the pathophysiology of myocardial ischemia and reperfusion injury in a clinically applicable 4-stage scheme.
Although it is premature to apply the classification immediately to guide clinical treatment at this time, this proposed classification could help incorporate the stages of tissue injury into clinical care for future patient risk assessment, management, and documentation.
The classification provides outcome measures and endpoints for MI research at the clinical and health systems level. It provides the fundamental framework for the development of future therapies.
Not all MIs are the same and the best possible treatment may not be “one size fits all.” The best possible individualized treatment must take into account the underlying tissue pathology. The CCS classification of acute MI, as described, could be instrumental in facilitating the development of such treatments and ultimately assist with the provision of personalized, differentiated, and targeted care for tissue injuries in the future. It can facilitate myocardial infarction research by providing the stages of myocardial infarction as useful outcome measures, clinical trial endpoints, and therapeutic targets.