Heart valve disease is a major source of cardiovascular morbidity and mortality worldwide.
Among the many recent advances are ( a ) greater recognition of the impact of atrial fibrillation (AF) on the development and evaluation of valvular disease, ( b ) new strategies for the global prevention of rheumatic heart disease (RC), ( c ) improved understanding and treatment of secondary mitral regurgitation (SMI), ( d ) an updated classification of bicuspid aortic valve disease (BAV), and ( e ) recognition of the increased cardiovascular risk associated with aortic stenosis (AS) moderate.
Additionally, with an aging population and the emerging epidemic of both degenerative and functional valvular heart disease, more transcatheter therapies are becoming available and are being actively investigated through rigorous clinical trials. This review provides an update on these topics with a focus on recent evidence and future directions.
| Global changes in the epidemiology of heart valve disease |
atrial fibrillation
A heart in which AF occurs is phenotypically characterized by larger atria, increased pulmonary vascular resistance, right heart failure, decreased forward flow, decreased cardiac output reserve, and increased pericardial containment, all of which contribute to adverse outcomes.
AF shares common cardiovascular risk factors implicated in degenerative valvular disease, including, but not limited to, advanced age, hypertension, diabetes, and hyperlipidemia. Therefore, the prevalence of AF in rheumatic or non-rheumatic valvular disease is very high, especially among those with moderate to severe valvular disease.
Complications of coexisting AF in patients with valvular disease include an increased risk of stroke and systemic embolization, as well as an increased risk of cardiovascular and all-cause mortality.
Rheumatic heart disease: prevention and treatment
CR is a consequence of rheumatic fever (RF) caused by a group A strep throat infection. Risk factors for high-incidence group A strep infections include poverty and limited access to health care. Improvements in socioeconomic status and access to adequate health care, which reduce the risk of transmission and infection by group A streptococci, as well as early and timely recognition and treatment of such infections, substantially reduce the incidence of RF and are the cornerstone of primary care.
Secondary prevention, aimed at preventing recurrence of RF and progression of established CR, is achieved by benzathine penicillin G administered intramuscularly every 3 or 4 weeks, but access to this medication has been very difficult in endemic areas, due in part to the decreased supply of the medication. Mitral balloon valvoplasty and valve repair/replacement are necessary for symptomatic severe CR, but for these interventions resources are also scarce where RF and CR are endemic.
Rheumatic mitral stenosis is the most common underlying valvular disease in patients in low- and middle-income countries who present with atrial fibrillation.
There is an intense renewed commitment by the World Health Organization, the World Heart Federation, and the American Heart Association, among other international and global organizations, to prevent and control RF and CR, given the persistence of these diseases. in low- and middle-income countries.
| Secondary mitral regurgitation: pathophysiology and management |
Traditionally, MSI has been considered a disease of the left ventricle (LV), with regional wall motion abnormalities leading to leaflet motion block and incomplete coaptation in patients with normal or near-normal mitral valve leaflets. ( Figure 1 ). The situation, however, is more complex due to the heterogeneity of the IMS.
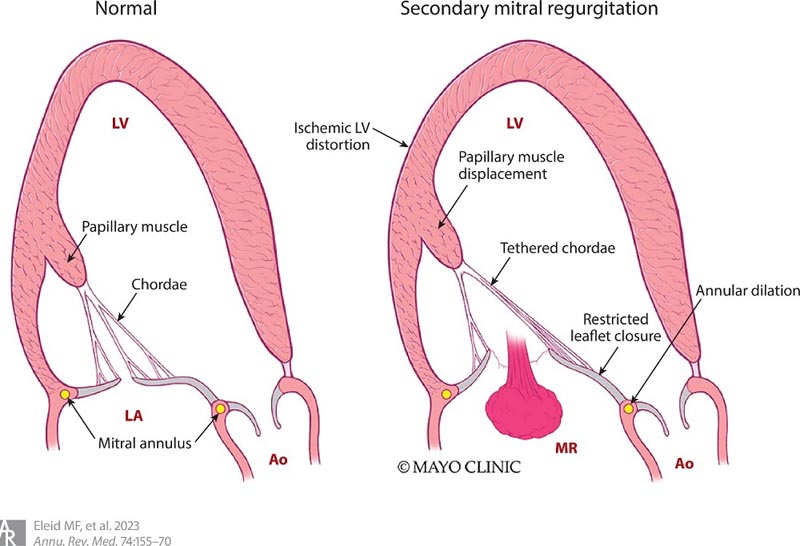
Figure 1 . The pathophysiology and mechanisms of secondary mitral regurgitation include left ventricular dilation resulting in displacement of the papillary muscle, tethering of the chordae, and restricted closure of the leaflets, as well as enlargement of the left atrium and mitral annulus. Abbreviations: Ao, aorta; LA, left atrium; VI, left ventricle; MRI: mitral valve insufficiency.
At one end of the spectrum is MSI with LV dilation leading to global distortion of mitral valve apparatus function and, in particular, annular dilation. In this situation, mitral regurgitation is essentially a bystander and the primary goal of treatment is to address LV dysfunction and reduce its size. Conversely, pathological processes affecting the ventricular myocardium may disproportionately involve segments supporting the mitral valve apparatus by causing leaflet immobilization and subsequent thickening and dysfunction.
From a therapeutic point of view, there are several issues to address. Since LV dysfunction (both global and regional) is an integral component of MSI, it should be addressed using guideline-determined pharmacological approaches and perhaps cardiac resynchronization therapy in highly selected patients.
In patients with coronary artery disease, revascularization alone has had an inconsistent effect on the severity of MR. The problem in patients with IMS undergoing coronary artery bypass grafting (CABG) is more nuanced; It has not been completely resolved whether CABG alone or CABG with mitral valve repair or replacement should be performed, particularly in patients without symptoms of heart failure.
For patients undergoing CABG in whom MSI is present but not considered the cause of symptoms, options include CABG alone, CABG plus mitral valve repair or preferably replacement, or CABG alone followed by close observation with the option of a percutaneous procedure.
In patients with symptomatic MSI, it is important to consider whether the symptoms are secondary to congestion (i.e., dyspnea) or perhaps secondary to low cardiac output (fatigue) as a consequence of the severity of LV dysfunction, remodeling, and scarring. and whether the degree of MI is proportional or disproportionate to the degree of
LV dilation ( figure 2 ). What is certain is that the percutaneous and surgical treatment of MSI is evolving and is currently the focus of a rapidly expanding technological arsenal.
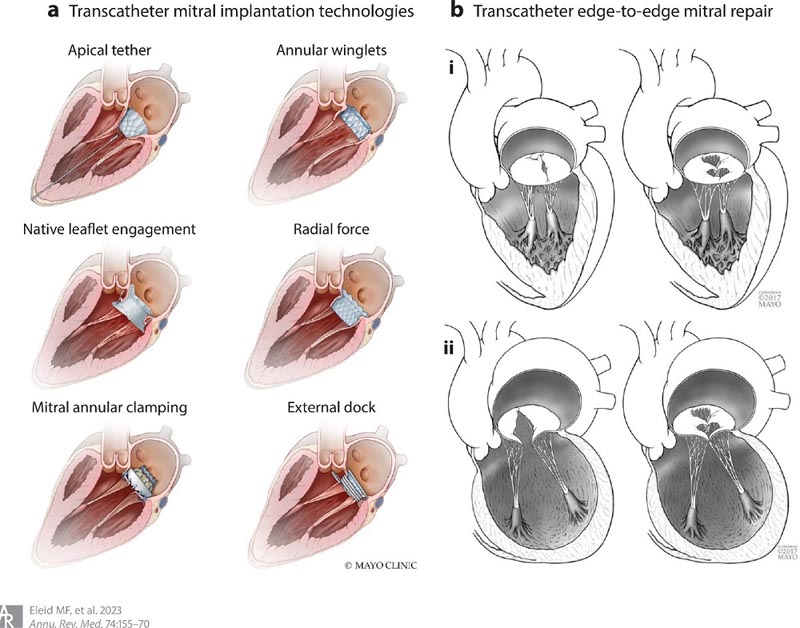
Figure 2 . (a) Percutaneous mitral valve implantation devices and their respective anchoring mechanisms. (b) Transcatheter edge-to-edge repair of the mitral valve in primary (i) and secondary (ii) mitral regurgitation.
The etiological association of AF/flutter with mitral regurgitation is not in dispute. However, what we do not know is what proportion of patients with incident AF/flutter and without preexisting heart valve disease at the time of diagnosis will develop significant valvular abnormalities. This issue is the subject of ongoing studies, which should help clarify the magnitude of the problem.
| Interventional Approaches for Mitral Valve Disease |
Mitral regurgitation is divided into primary and secondary etiologies, which are very important in deciding the optimal treatment.
Primary mitral valve disease includes degenerative etiologies such as fibroelastic deficiency and mitral valve prolapse, which are more commonly found in high-income countries, while rheumatic mitral valve disease is more common in low- and middle-income countries. Endocarditis and calcific mitral valve disease are other important causes of primary mitral valve disease.
Surgical mitral valve repair is the intervention of choice for patients with severe primary MR who have adequate mitral valve anatomy. However, many patients lack adequate anatomy for repair or are at increased risk of mortality from cardiac surgery due to age, comorbidities, or technical impairments. For these patients, an increasing number of transcatheter therapies are being used to address a wide range of mitral valve diseases.
Transcatheter mitral valve implantation is a novel, minimally invasive treatment strategy for patients with severe mitral valve disease at high risk for surgery, as well as for patients with calcific mitral stenosis due to calcification of the mitral annulus. Transseptal implantation of transcatheter balloon-expandable valves for patients with degenerated mitral bioprostheses after initial refinement of the procedure has become a safe and effective procedure approved by the US Food and Drug Administration (FDA).
| Aortic stenosis: hemodynamic subsets and new therapeutic indications |
Transcatheter aortic valve implantation
Since the initial human procedure 20 years ago, transcatheter aortic valve implantation (TAVI) has undergone rich and rigorous development through interdisciplinary collaboration and randomized clinical trials to become a common and highly effective therapy. Initial studies of TAVI in patients at high or prohibitive risk for surgery established the feasibility of the procedure but identified areas for improvement, including paravalvular leak (PVL) and risk of vascular complications.
These complications are now rare with TAVI thanks to improvements in device technology, procedural technique, CT-based planning, and patient selection. TAVI is now a first-line therapy for AS patients at intermediate or higher risk for surgical aortic valve replacement
TAVI is currently recommended as a class I indication in the recent heart valve disease guidelines from the American Heart Association and the American College of Cardiology for patients with AS who are at low risk for surgical aortic valve replacement and are appropriate candidates for biological prosthesis with a life expectancy of 20 years. years or less
Moderate aortic stenosis
Recent data in contemporary practice suggest an unfavorable prognosis in patients with moderate AD; Some data suggest similarly high mortality associated with moderate and severe AD when untreated, but it is unclear whether the increased mortality was related to comorbidities.
Increased mortality has been associated with reduced LVEF (<50%), diastolic dysfunction, clinical heart failure, abnormal global LV strain, and elevation of N-terminal pro b-type natriuretic peptide . Clinical trials examining TAVI versus guideline-directed medical treatment in patients with symptomatic moderate AS are ongoing.
Low gradient aortic stenosis
The basic determinants of the mean gradient across the aortic valve are area and direct flow. A small aortic valve area (≤1 cm2), associated with a low gradient (<40 mm Hg) and peak velocity (<4 m/sec), defines low gradient aortic stenosis (LGAS). LGAS typically occurs as a result of low forward flow, assuming no measurement errors, or high transvalvular afterload (i.e., systemic hypertension). Any condition that results in low direct flow can result in LGAS. Treatment of systemic hypertension in LGAS is associated with a reduction in LV filling pressures and an increase in forward flow, and is recommended as an important step in treatment.
Bicuspid aortic valve
BAV disease is the most common congenital heart disease, affecting 1-2% of the general population. Genetic determinants of BAV disease also contribute to aortopathy, present in 50% of patients with BAV disease and characterized by reduced structural integrity and elasticity of the aortic wall.
Abnormal flow dynamics through a BAV, especially when associated with progressive stenosis or regurgitation, also contribute to aortic dilation. The most common phenotypes are fusion of the right and left coronary cusps, followed by fusion of the right and non-coronary cusps.
| Tricuspid valve regurgitation |
Time of intervention
Current guidelines recommend tricuspid valve intervention in primary tricuspid regurgitation (TR) when there are symptoms or when there is at least progressive right ventricular (RV) dilation or systolic dysfunction, or when there is significant TR or annular dilation. tricuspid when undergoing open heart surgery for left-sided heart disease.
TR remains largely undertreated, and the recent slightly upward trend in tricuspid valve surgery for TR, especially repair, has also been associated with older patient age and comorbidities at the time of surgery. More precise quantitative measurements of RV size and systolic function (e.g., 3D echocardiography or cardiac MRI) and identification of earlier triggers for tricuspid valve surgery are being actively investigated to improve outcomes.
Transcatheter tricuspid interventional approaches
Only 10% of patients with severe symptomatic TR undergo surgical treatment, while the majority are treated with diuretic treatment alone. Given the adverse impact of severe TR on both quality of life and survival, and the extreme degree of TR observed in a large proportion of patients, there is a great need for minimally invasive transcatheter therapies.
Numerous transcatheter therapies are being studied, including edge-to-edge leaflet repair with devices, which have demonstrated favorable safety and efficacy in reducing the severity of TR by two or more degrees in most patients. Important questions to be addressed in future studies include the optimal timing of intervention, the ideal combination of various devices with specific anatomy, and the long-term benefit and durability of these treatments.
| Paravalvular leak: scope of the problem and interventional management |
Paravalvular leak (PVL) is a condition that compromises the prosthetic valves and is characterized by regurgitation of blood around the prosthesis.
In surgical prosthetic valves, PVL may be due to tissue friability in conditions such as endocarditis and steroid use, or to annular calcification. PVL affects 2% to 10% of prosthetic aortic valves and 7% to 17% of prosthetic mitral valves. In TAVI, PVL rates have decreased dramatically over the past 10 years due to improvements in device technology and CT-based sizing techniques.
Moderate or severe PVL can lead to symptoms of heart failure, while any degree of PVL can lead to hemolytic anemia due to mechanical damage to red blood cells through shear forces. The AHA/ACC valvular heart disease guidelines recommend percutaneous PVL closure for patients who have attributable symptoms, adequate anatomy, and a high risk for cardiac surgery.
| Future directions |
Despite extraordinary advances in the treatment of valvular heart disease, a large number of questions and treatment gaps remain.
Ongoing clinical trials will provide important evidence to inform questions about (a) earlier intervention for moderate AS and asymptomatic severe AS, (b) transcatheter mitral valve implantation in patients with mitral regurgitation as well as in those with calcific diseases of the the mitral valve, (c) anticoagulation strategies in cardiac valvular disease, and (d) transcatheter intervention in patients with severe TR.
Early-stage trials of new transcatheter valve repair and replacement devices to test safety and efficacy are still needed to address the growing population of patients with severe valvular disease. Future studies are also needed to better understand the pathophysiology of calcific valve disease and explore the feasibility of tissue engineering in the development of new prosthetic heart valves, the role of artificial intelligence in the detection and timing of treatment of valve disease. .
















