| The prevalence of people with asthma among COVID19 patients is similar to the global prevalence of asthma. People with asthma are not at increased risk of acquiring COVID-19 and have similar clinical outcomes to patients without asthma. |
As COVID-19 continues to spread around the world with devastating impact, there are concerns that people with asthma are at higher risk of contracting the disease or worse outcomes. This is based on three main factors.
- First, people with chronic respiratory conditions such as asthma were historically reported to be at increased risk compared to their counterparts during Middle East Respiratory Syndrome (MERS), caused by a virus with close sequence homology to SARS. -CoV-2. Therefore, it seemed likely that this would also be the case for COVID-19.
- Second, viral respiratory infections such as coronaviruses are powerful triggers of asthma exacerbations.
- Finally, inhaled and oral corticosteroids, a key treatment for persistent asthma and acute exacerbations, respectively, may increase susceptibility to and severity of COVID-19 infection.
While these theories seem plausible, there is limited evidence to support them.
Current evidence shows that asthma is not among the top 10 comorbidities associated with COVID-19 deaths, with obesity, diabetes and chronic heart disease being the most frequently reported.
This is consistent with trends observed during the SARS-CoV-1 epidemic. Early reports from Wuhan in China suggest that asthma is underrepresented compared to population prevalence. However, the US Center for Disease Control (CDC) has reported that among younger patients hospitalized with COVID-19, obesity, asthma and diabetes were the most common comorbidities.
There have been recommendations from various government agencies around the world advising people with asthma to be more cautious and isolate themselves for longer, affecting their livelihood, mental health and quality of life. People with asthma were reported to have a higher prevalence of anxiety and stress than controls without asthma.
A qualitative study conducted in the United Kingdom among patients with respiratory diseases, including asthma, reported that they were afraid of dying if they became infected with COVID-19 and were confused by the conflicting messages about the protection they received. Furthermore, despite this advice, evidence for longer durations of self-isolation for people with asthma is scarce.
Aim
This systematic review aimed to summarize the evidence on the risk of infection, severe illness and death from COVID-19 in people with asthma.
Data sources and study selection
A comprehensive search of electronic databases was conducted, including preprint repositories and the WHO COVID-19 database (up to May 26, 2020). Studies that reported COVID-19 in people with asthma were included. For binary outcomes, we performed a Sidik-Jonkman random-effects meta-analysis. We explored quantitative heterogeneity using subgroup analysis, meta-regression, and evaluation of the I2 statistic.
Results
57 studies were included with an overall sample size of 587,280 .
The prevalence of asthma among people infected with COVID-19 was 7.46% (95% CI = 6.25–8.67). Non-severe asthma was more common than severe asthma (9.61% vs. 4.13%).
Pooled analysis showed a 14% risk ratio reduction in acquiring COVID-19 (95% CI = 0.80–0.94; p < 0.0001) and a 13% reduction in hospitalization with COVID-19 (95% CI = 0.77–0.99, p = 0.03) for people with asthma compared to those without.
There was no significant difference in the combined risk of requiring ICU admission and/or receiving mechanical ventilation for people with asthma (RR = 0.87; 95% CI = 0.94-1.37; p = 0.19) and the risk of death from COVID-19 (RR = 0.87; 95% CI = 0.68-1.10; p = 0.25).
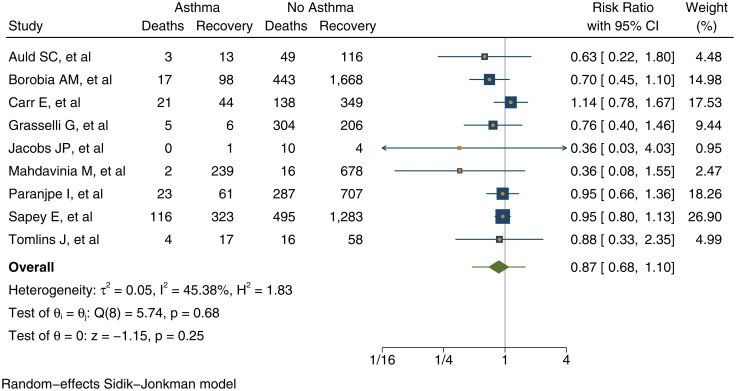
Risk of death versus recovery from COVID-19 among people with asthma compared to those without asthma.
Discussion
This systematic review aims to assess the vulnerability of people with asthma during the COVID-19 pandemic. The results revealed an asthma prevalence of 7.46% among those who tested positive for COVID-19. Although these studies come from countries with different asthma prevalence, overall this combined prevalence is similar to the self-reported asthma symptom prevalence of 8.6% .
In studies that reported asthma severity, we found that non-severe asthma among people with COVID-19 was more common than severe asthma (9.6% vs. 4.13%) as in most populations .
We found a 14% (95% CI = 0.80–0.94) lower risk of contracting COVID-19 in people with asthma, which is an absolute reduction of 50 cases per 1000 people. This is consistent with the trend observed during the SARS pandemic. There are several possible explanations for this reduced risk, including the observation that people with high T2 asthma have downregulated angiotensin-converting enzyme-2 (ACE-2) receptors that may reduce their risk of SARS infection. -CoV-2.
Preliminary evidence from the Severe Asthma Research Program-3 has shown that inhaled corticosteroid (ICS) therapy , the main treatment modality in asthmatics, is associated with lower expression of ACE-2 (one of the binding sites for SARS-CoV-2). This may confer a reduced vulnerability to COVID-19 and the development of less severe illness.
Increasing age is strongly associated with an increased risk of acquiring COVID-19 among asthmatics and explains 70% of the variance between studies in our analysis. This is an expected finding and in line with other COVID-19 studies showing age as one of the most important predictors of COVID-19 vulnerability and prognosis.
Increasing age is not statistically associated with an increased risk of mechanical ventilation in people with asthma. One study reported that asthma prolonged intubation time in patients <65 years, suggesting that asthma has a greater impact on the course of COVID-19 in younger people.
On the other hand, a recent study in Spain among asthmatics reported that those who acquired COVID-19 were older with a higher prevalence of comorbidities compared to those who were COVID-19 negative. It was also reported that older people and those with comorbidities were more likely to be hospitalized. Of note, a low hospitalization rate among people with COVID-19 of 0.23% was reported in this study.
There is no evidence of a difference in the risk of death from COVID-19 for people with asthma (RR = 0.87, 95% CI = 0.68 to 1.10, p = 0.19).
A study in New York also reported that asthma was not associated with mortality (87). We observed that the average age of the grouped studies was 52 years. As previous studies have shown that the case fatality rate increases substantially above 50 years of age, our findings could present a conservative estimate of the possible reduction in the risk of death.
Finally, a proportion of COVID-19 patients experience prolonged effects after acute illness, now termed "long COVID" . The more common symptoms of fatigue, shortness of breath, and cough may be more likely or prominent in people with underlying airway disease. Although beyond the scope of this analysis, it will be crucial to examine these risks in additional studies of people with asthma and COVID-19.
In summary , the findings of this study suggest that the prevalence of people with asthma among COVID-19 patients is similar to the global prevalence of asthma. Overall findings based on available evidence suggest that people with asthma are not at increased risk of acquiring COVID-19 compared to those without asthma and have similar clinical outcomes.
More high-quality primary studies and data sharing on asthma and COVID-19 are needed globally to improve our understanding of how SARS-CoV-2 affects people with asthma.
Conclusion The findings of this study suggest that the prevalence of people with asthma among COVID-19 patients is similar to the global prevalence of asthma. The overall findings suggest that people with asthma have a lower risk than those without asthma of acquiring COVID-19 and have similar clinical outcomes . |
















