Summary
|
Introduction
Abdominal aortic aneurysm (AAA) is a multifactorial vascular disease with high mortality (estimated in the region of 200,000 deaths per year worldwide) that is related to advanced age and is more common in men than women.
The prevalence of AAA in selected population studies is very different: it is higher among men and lower among women in different studies. The overall pooled prevalence of AAA across 56 studies was found to be 4.8% . The prevalence of AAA is higher in Australia (6.7%) than in Europe (2.5%) and America (2.2%); the lowest prevalence is found in Asia (0.5%).
AAAs are usually located below the renal arteries and end before the bifurcation of the aorta (Figure 1).
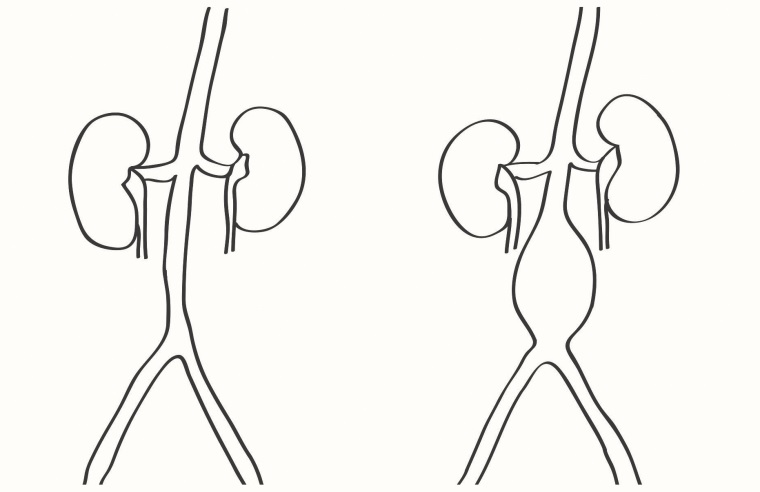
Figure 1. Location of the abdominal aortic aneurysm (author’s drawing).
The development of diagnostic tools and screening programs in recent years has promoted more frequent and earlier detection of AAA.
The course of the disease is long and may be asymptomatic for many years. For this reason, undiagnosed AAAs will, over time, result in a fatal rupture in most cases. This dramatic sequence of events dictated by the natural history of AAA requires careful monitoring of patients in high-risk groups.
Risk factor’s
The main risk factors for the development of AAA are smoking, hypertension, advanced age, male sex, atherosclerosis, dyslipidemia, positive family history, and hereditary predisposition.
In a large cross-sectional study published in February 2020 (1.5 million women and 0.8 million men), it was shown that in women <75 years of age, the risk of AAA is much higher than previous studies had indicated .
- Compared with never smoking, current smoking was associated with a 15-fold increased risk of AAA among women and a 7-fold increased risk among men.
- Each additional 4.0 kg/m2 higher body mass index (BMI) point was associated with a 14% increased risk of AAA and was similar in men and women.
- Each 12.9 mmHg higher systolic blood pressure was associated with a 22% increased risk and this was somewhat stronger in women than in men.
In the case of a thoracic aortic aneurysm , genetic data can be used to identify certain people at risk. In the case of an AAA, the role of genetic factors is less than in the case of thoracic aortic aneurysms. Marfan syndrome and Ehlers-Danlos syndrome have also been strongly associated with AAAs. Other causes of AAA development include trauma, infection, and arteritis.
Much evidence shows that smoking is the main and strongest predictor of AAA prevalence, growth, and rupture rates. This is directly related to the number of years of smoking and decreases with the number of years after quitting. The risk of developing an AAA is particularly high in people who have smoked more than 20 cigarettes a day for many years.
The risk factors for the development of AAA are not strictly identical to the risk factors for rupture.
Risk factors for the development of AAA are male sex, current or past smoking, hypertension, inflammation of the aortic wall, and atherosclerosis. Risk factors for AAA rupture are female sex, mean arterial pressure, current or past smoking, reduced forced expiratory volume in one second (FEV1), and aneurysm diameter greater than 5.0 cm. Attention should be paid not only to the treatment of classic risk factors such as hypertension and hyperlipidemia, but also to the monitoring of selected biomarkers .
Biomarkers such as white blood cell count, fibrinogen, D-dimer , troponin T, N-terminal probrain natriuretic peptide, and C-reactive protein may also be useful in assessing the risk of AAA. These biomarkers are an early sign of the development of inflammation and oxidative stress .
These changes alter the normal functioning of the vascular wall, which can promote the development of aneurysms in the future. The Atherosclerosis Risk in Communities (ARIC) study showed that higher concentrations of these biomarkers were associated with an increased risk of AAA.
Pathophysiology
The aorta is a type of elastic artery, made up of three layers (internal, medial and external), whose structure changes in its different parts. The middle layer of the aorta, which is the thickest, is made up of elastic fibers and vascular smooth muscle cells. There are more layers of elastic fibers in the thoracic section, and their number decreases in the abdominal section of the aorta. This difference in the structure of the aorta wall is one of the reasons why aneurysms are more common in the abdominal part of the aorta.
The aortic wall in older people is characterized by thinning, impaired vascular endothelial function, and reduced elastin fibers. These changes cause dilation of the aortic lumen and can lead to the formation of aneurysms.
In addition to the dimension from which the risk of AAA rupture is predicted, other parameters such as the distribution of vascular wall tension, the degree of asymmetry, the presence of intraluminal thrombus, and the expansion rate are also important.
Screening programs
AAAs remain asymptomatic for many years. They are four to six times more common in men than in women and the risk of the disease increases after age 60; Women develop the disease approximately 10 years later than men.
The prevalence of AAA is higher in first-degree relatives compared to the general population, regardless of sex, so abdominal ultrasound is recommended in siblings of patients with AAA.
Among the 379 siblings examined, AAA were found in 14% (Norrbotten County) and 17% of siblings (Stockholm County); the prevalence among sisters was 6% in both regions. The factors associated with a higher risk of AAA among siblings were male sex and age > 65 years; Smoking was not statistically significant as a risk factor in these groups.
AAAs are discovered as a pulsating abdominal mass on routine physical examination or as an incidental finding on ultrasound, abdominal CT, or MRI performed for other purposes.
Expanding AAAs can become painful , causing throbbing sensations in the abdomen or pain in the chest, lower back, and scrotum. Most AAAs are asymptomatic to patients and are detected accidentally. For these reasons, screening tests have some importance in the diagnosis of AAA.
The first screening programs were dedicated to older men who smoked cigarettes and had high blood pressure. In subsequent years, screening programs for older women were also carried out.
The largest screening programs related to AAA are the Multicentre Aneurysm Screening Study (MASS) (n = 67,800), the Viborg County Screening Trial, Denmark (n = 12,639) [16], the Chichester Screening Trial , United Kingdom ( n = 15,382), the Western Australian Screening Trial ( n = 38,480) and the Regional Veterans Affairs Health Care System screening program ( n = 6,142).
The prevalence of AAA among men in screening programs ranged from 4.0% to 7.6% and the majority of aneurysms detected were small (≤4 to 4.5 cm).
Only 0.3% to 0.6% of patients examined had AAAs of 5.5 cm or more in diameter. The Viborg trial and the Western Australian trial looked at mortality in screened men by age at screening.
In the Viborg trial, the reduction in mortality risk was similar for men aged 64 to 65 years versus those aged 66 to 73 years. Similarly, in the Western Australian trial, the death rate in examined men aged 65 to 74 years versus men aged 64 to 83 years was similar.
The Chichester trial also included screening women aged 65 to 80 years and found a low prevalence of AAA in this population. Aneurysms were detected in 1.3% of the women examined; the diameter in 75% of cases ranged between 3.0 cm and 3.9 cm. Rupture rates among men and women were 0.2% in both groups.
Invitation to screening results in reduced mortality: it has been estimated that inviting 305 men for screening prevents one death from ruptured AAA. It has also been estimated that inviting 1,000 men to participate in a screening ultrasound of the abdomen prevents two emergency surgeries for a ruptured aneurysm.
Based on analysis of screening program results published in 2019, the U.S. Preventive Services Task Force’s December guidelines do not recommend routine screening for men and women who have never smoked cigarettes.
In men 65 to 75 years of age who have smoked cigarettes, a single screening test is recommended; in women in the same group, a screening test may be considered.
Bown et al. analyzed the performance of follow-up examinations in patients diagnosed with small AAAs (diameter <5.5 cm). The authors included in the analyzes 18 studies containing records of 15,471 patients (13,728 men and 1,743 women).
Most small AAAs grow slowly, but there is substantial variation in growth rates between different individuals. The mean growth of small 3.0 cm AAAs in men was 1.28 mm per year , while the mean annual growth of larger aneurysms (with a diameter of 5.0 cm) was 3.61 mm; smokers have a higher growth rate.
Among women, the risk of rupture for all AAA sizes was four times higher than in men.
Conclusions Prevention of AAA should be of utmost importance because potential drug treatments for aortic aneurysms are still in the clinical trial phase. We can achieve the prophylactic goal through careful monitoring and treatment of cardiovascular risk factors. This strategy can be extended to older people (especially older men who smoke cigarettes) with a screening test, i.e. abdominal ultrasound. The golden rule that "prevention is better than cure" works very well in relation to the natural history of AAA. |
















