This series will address the most common painful foot and ankle disorders. Morton’s neuroma, plantar fasciitis, and Achilles tendinopathy are among the most common painful conditions of the foot and ankle. The review summarizes current evidence on the epidemiology, pathophysiology, diagnosis and non-surgical treatments of these conditions.
1. Morton’s neuroma
Morton’s neuroma , which consists of interdigital neuronal thickening and fibrosis, is characterized by burning pain in the sole of the foot and numbness or burning pain that may radiate to the affected toes (commonly the third and fourth toes). First-line nonsurgical treatment consists of reducing activities that cause pain, bracing, and interdigital injection of corticosteroids; however, approximately 30% of patients may not respond to conservative treatment.
Box Questions and Answers for Doctors on Common Foot and Ankle Conditions Should patients with suspected Morton’s neuroma undergo imaging studies? The diagnosis of Morton’s neuroma is based primarily on history and physical examination. Patients often report pain when walking, pain with tight shoes, pain improvement with rest, and pain when stretching the toes. On clinical examination, the doctor may provoke pain with palpation of the affected web space and positive Mulder and Tinel signs. Imaging, including radiographic, MRI, and ultrasound, is primarily used to rule out other pathologies. Should patients with Morton’s neuroma receive corticosteroid injections? Corticosteroid injections are an option for non-surgical treatment of Morton’s neuroma, although they may only provide short-term pain relief. Complications are rare; Approximately 30% of patients may ultimately undergo surgery after the injection. No difference in efficacy has been demonstrated between ultrasound-guided and non-ultrasound-guided injections. |
Morton’s neuroma
Definition and pathophysiology
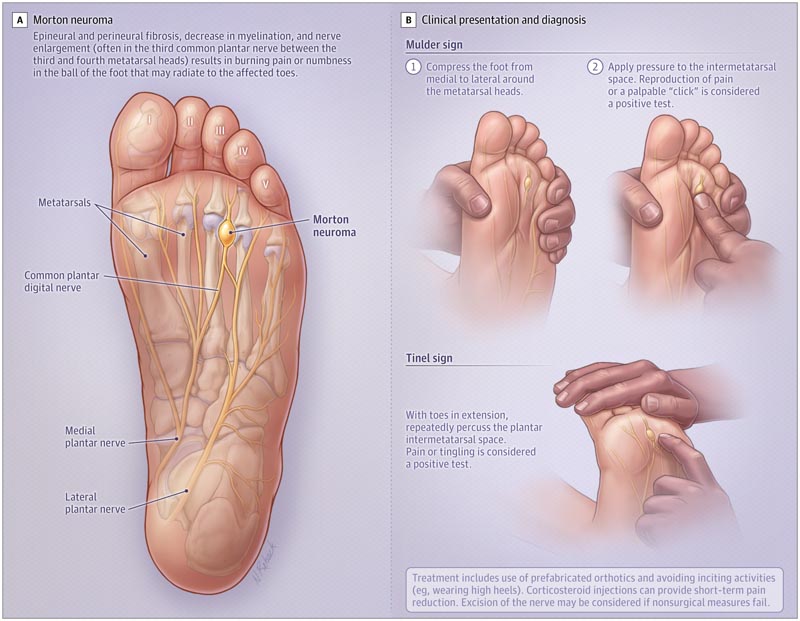
Morton’s neuroma, also known as interdigital neuroma , most commonly affects the third digital nerve of the foot, often causing neuropathic pain in the affected toes (Figure 1 A).
Histologically, Morton neuromas are neither nodules nor tumors , but are characterized by epineural and perineural fibrosis and decreased myelination and enlargement of the nerves compared to autopsy controls. A clear etiology has not been demonstrated.
Epidemiology
The incidence of Morton’s neuroma is unknown, but it is the second most common compressive neuropathy (carpal tunnel syndrome is the most common compressive neuropathy). Patients usually present between 45 and 54 years of age. Of patients undergoing surgical excision, the female-to-male ratio was greater than 4:1. The third interdigital nerve is affected in up to 87% of cases, followed by the second nerve in the rest of the cases. Morton’s neuroma occurs bilaterally in 21% of patients.
Clinical presentation and diagnosis
Morton’s neuroma can be diagnosed based on medical history and physical examination. Patients often present with burning pain between the metatarsal heads on the plantar aspect of the foot. The pain may radiate to the two adjacent fingers and patients may report numbness or “electrical sensations” in the fingers.
Wearing tight shoes or high heels can exacerbate symptoms. Among patients undergoing excision for Morton neuroma, 91% report exacerbation with walking, 86% report pain worsening with tight shoes, 81% report pain relieved with rest, and 79% report pain by stretching the toes.
Physical examination usually shows pain when compressing the affected space (index finger compression test), Mulder’s sign, and Tinel’s sign (Figure 1 B). Among patients undergoing surgical procedures for clinically diagnosed Morton’s neuroma, 97.5% (95% CI, 95%-100%) have histologically proven Morton’s neuroma.
The diagnosis can usually be made based on history and physical examination. Radiographic imaging of the standing foot may be performed to evaluate other conditions, such as stress fracture or avascular necrosis of the metatarsal head.
Ultrasound should be used to identify a hypoechoic mass in the metatarsal heads or magnetic resonance imaging (MRI) can be performed when the clinical diagnosis alone is inconclusive. A systematic review found no significant difference between ultrasound (sensitivity 91% [95% CI, 83%-96%] and specificity 85% [95% CI, 41%-100%]) versus MRI (90% sensitivity [95% CI, 82%-96%] and 100% specificity [95% CI, 73%-100%]) to diagnose Morton’s neuroma.
Treatment
Initial conservative treatments for Morton’s neuroma involve avoiding strenuous activities and modifying shoes to reduce pressure. Shoes with a wide toe and more cushioning can relieve symptoms, and pre-made orthotics with pads can be added for metatarsals or neuromas. High-heeled shoes should be avoided. Custom foot orthoses can relieve pain in some patients with Morton’s neuroma.
In a randomized double-blind trial, 72 participants were assigned to receive custom-made insoles (with longitudinal arch support and support just behind the metatarsal heads) or non-customized flat insoles, and then were re-evaluated for pain when walking (based on a visual analogue scale) for pain ranging from 0 [no pain] to 10 [unbearable pain]). After 24 months, those assigned to receive custom insoles experienced greater pain relief from baseline, although both groups improved (pain score decreased from 5.8 to 2.7 for custom insoles and from 6.1 to 4. 7 for non-personalized templates; P = 0.048).
Corticosteroid injection may provide short-term (1 week to 3 months) pain reduction in Morton’s neuroma. The benefit of corticosteroids was quantified in a blinded randomized trial of 131 patients comparing a single injection of methylprednisolone mixed with local anesthetic versus local anesthetic alone. The steroid group demonstrated better improvement in the patient’s global assessment of the foot health scale at 3 months (VAS ranging from 0 [worst imaginable foot health] to 100 [best imaginable foot health]; mean difference , 14.1 points [95% CI, 5.5 -22.8]; p = 0.002).
In a systematic review of 469 patients who underwent ultrasound-guided corticosteroid injection, 140 (29.85%) ultimately underwent surgical treatment, usually due to severe pain that limited walking. 10 If the pain is severe or does not relieve after 6 weeks of conservative treatment, referral to a specialist surgeon is warranted. Surgical treatment usually involves removing the common interdigital nerve (neurectomy), with a pain reduction of more than 95% (measured by VAS score).
Complications of treatment
Adverse effects associated with corticosteroid injections for Morton’s neuroma include skin whitening (3.4%) and skin atrophy (5.88%). Surgical complications of neurectomy include neuroma formation at the end of the cut nerve (3%-8%), which can cause persistent pain in the sole of the forefoot.















