Compelling evidence in The American Journal of Pathology points to the cytoprotective and proregenerative effects of a neuropeptide in promoting corneal healing after ocular injury.
Summary Corneal endothelial cells (CEnC) regulate corneal hydration and maintain tissue transparency through their barrier and pump function. However, these cells exhibit limited regenerative capacity after injury. Currently, corneal transplantation is the only established therapy to restore endothelial function and there are no pharmacological interventions available to restore endothelial function. This study investigated the efficacy of the neuropeptide α-melanocyte-stimulating hormone (α-MSH) in promoting endothelial regeneration during the critical window between ocular injury and the onset of endothelial decompensation using an established murine model of transcorneal freeze injury. Local administration of α-MSH after injury prevented corneal edema and opacity, reduced leukocyte infiltration, and limited CEnC apoptosis while promoting its proliferation. These results suggest that α-MSH has a proregenerative and cytoprotective function in CEnCs and shows promise as a therapy for the prevention and treatment of corneal endothelial dysfunction. |
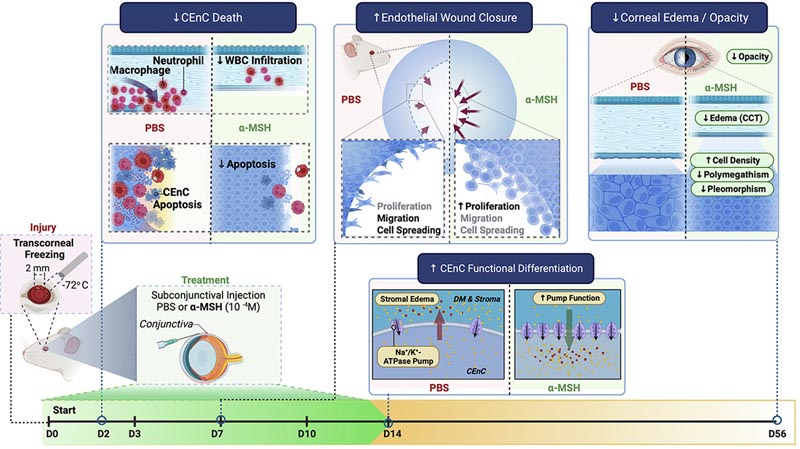
Graphical abstract : Harvard Medical School researchers have demonstrated the potent therapeutic effects of administration of the neuropeptide α-melanocyte-stimulating hormone (α-MSH) through melanocortin receptor agonism, providing compelling evidence for the therapeutic potential of this route for a wide range of eye diseases. CEnC, corneal endothelial cells; PBS, phosphate-buffered saline (Credit: The American Journal of Pathology ).
Comments
Findings from a pioneering study published by Elsevier reveal that administration of the neuropeptide α-melanocyte-stimulating hormone (α-MSH) promotes corneal healing and restores normal ocular function to an otherwise degenerated and diseased cornea. , providing protection against cell death and promoting cell regeneration.
Due to the lack of medical treatment currently available, patients suffering from corneal endothelial disease , which causes inflammation of the cornea and potentially blindness, commonly require a corneal transplant. In fact, corneal transplant is the most common type of transplant performed.
There is an urgent and unmet need for safe and effective medical strategies for the prevention and reversal of persistent corneal edema, according to Mass Eye and Ear researchers in the Department of Ophthalmology at Harvard Medical School. Therefore, there is a pressing need to develop an effective treatment to prevent and potentially reverse corneal edema due to loss of corneal endothelial cells (CenC) after corneal injury.
This study examined the effect of local administration of α-MSH on persistent corneal edema and endothelial regeneration in an established model of injury-induced endothelial decompensation. The results show the impressive therapeutic potential of promoting the melanocortin pathway using α-MSH, thus opening new avenues of therapy.
Principal investigator Reza Dana, MD, MSc, MPH, director of the Cornea and Refractive Surgery Service at Mass Eye and Ear, and Claes H. Dohlman Professor of Ophthalmology at Harvard Medical School, explains: "Our data, which demonstrate The potent therapeutic effects of α-MSH through melanocortin receptor agonism provide compelling evidence of the therapeutic potential of this pathway for a wide range of ocular disorders such as Fuchs’ dystrophy, a common disease and indication for corneal transplantation, as well as as other disorders of the corneal endothelium that lead to inflammation of the cornea.
α-MSH is an evolutionarily conserved neuropeptide derived from the proteolysis of proopiomelanocortin and exerts a variety of functions through different melanocortin receptors expressed in various tissues. The findings of this pivotal study show that administration of α-MSH:
- Prevents the death of corneal endothelial cells.
- Restores normal endothelial function.
- It allows the cornea to regain its normal thickness after a serious injury that normally causes corneal thickening.
- It causes corneal cells to regenerate.
Interventions to prevent corneal edema after ocular injury are currently limited to topical hypertonic saline and topical anti-inflammatory drugs. However, these interventions have limited efficacy and do not prevent CEnC decompensation.
Dr. Dana concludes: "The findings of our study suggest the therapeutic potential of α-MSH, or analogs that work by activating the melanocortin receptor system, in the treatment of pathologies where there is a risk of corneal endothelial dysfunction, such as corneal injury or intraocular surgery. This study describes the fundamental role that neuropeptides play in the maintenance of CEnC and offers a novel perspective on their potential application in corneal endothelial regeneration."
















