Iatrogenic Alzheimer’s disease in cadaveric pituitary-derived growth hormone receptors Summary Alzheimer’s disease (AD) is pathologically characterized by the deposition of amyloid beta (Aβ) in the brain parenchyma and blood vessels (as cerebral amyloid angiopathy (CAA)) and by neurofibrillary tangles of hyperphosphorylated tau. Compelling genetic and biomarker evidence supports Aβ as the underlying cause of AD. We previously reported human transmission of Aβ and CAA pathology in relatively young adults who had died of iatrogenic Creutzfeldt-Jakob disease (iCJD) after childhood treatment with cadaver-derived pituitary growth hormone (c-hGH) contaminated with CJD prions and Aβ seeds. This raised the possibility that c-hGH recipients who did not die from iCJD could eventually develop Alzheimer’s disease (AD). Here we describe recipients who developed dementia and biomarker changes within the phenotypic spectrum of AD, suggesting that AD, like CJD, has environmentally acquired (iatrogenic) forms as well as sporadic late-onset and late-onset inherited forms. early. Although iatrogenic AD may be rare and there is no indication that Aβ can be transmitted between individuals in activities of daily living, its recognition emphasizes the need to review measures to prevent accidental transmissions through other medical and surgical procedures. As propagating Aβ pools can exhibit structural diversity similar to that of conventional prions, it is possible that therapeutic strategies targeting disease-related pools could lead to selection of minor components and development of resistance. |
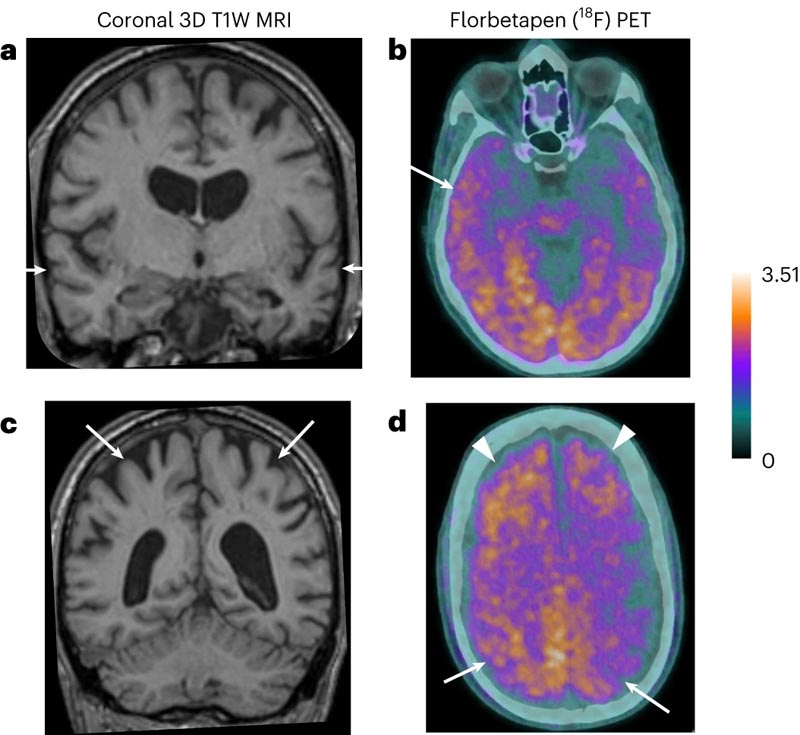
Image : a, Coronal high-resolution T1-weighted (T1W) three-dimensional (3D) magnetic resonance imaging (MRI) image through the temporal lobes demonstrates volume loss within the temporal lobes bilaterally (arrows) and also a marked central atrophy. b, Axial PET images demonstrate diffuse increased tracer uptake in the cortex and subcortical white matter, increased in the right temporal lobe compared to the left. c, Coronal high-resolution MR image (3D T1W) through the superior parietal lobes bilaterally demonstrating marked volume loss (arrows). d, Axial PET images demonstrate marked tracer uptake within the superior parietal lobes bilaterally (arrows), in addition to increased uptake in the frontal lobes bilaterally (arrowheads).
Comments
Alzheimer’s disease is caused by the amyloid beta protein and is usually a sporadic condition in late adult life or, more rarely, an inherited condition that occurs due to a defective gene. The new paper published in Nature Medicine provides the first evidence of Alzheimer’s disease in living people that appears to have been acquired medically and due to the transmission of the amyloid beta protein.
All of the people described in the article had been treated as children with a type of human growth hormone extracted from the pituitary glands of deceased individuals (cadaver-derived human growth hormone, or c-hGH). It was used to treat at least 1,848 people in the United Kingdom between 1959 and 1985, and was used for various causes of short stature. It was withdrawn in 1985 after it was recognized that some batches of c-hGH were contaminated with prions (infectious proteins) that had caused Creutzfeldt-Jakob disease (CJD) in some people. c-hGH was then replaced with a synthetic growth hormone that did not carry the risk of transmitting Creutzfeldt-Jakob disease (CJD).
These researchers previously reported that some patients with Creutzfeldt-Jakob disease (CJD) due to c-hGH treatment (called iatrogenic CJD) had also prematurely developed deposits of the amyloid beta protein in their brains. The scientists went on to demonstrate in a 2018 paper that archived samples of c-hGH were contaminated with the amyloid beta protein and, despite being stored for decades, transmitted amyloid beta pathology to laboratory mice when injected. They suggested that people exposed to contaminated c-hGH, who did not succumb to Creutzfeldt-Jakob disease (CJD) and lived longer, could eventually develop Alzheimer’s disease.
This latest article reports on eight people referred to the UCLH National Prion Clinic at the National Hospital for Neurology and Neurosurgery, London, who had been treated with c-hGH in childhood, often for several years.
Five of these people had symptoms of dementia and had already been diagnosed with Alzheimer’s disease or would meet the diagnostic criteria for this condition; another person met criteria for mild cognitive impairment. These people were between 38 and 55 years old when they began to present neurological symptoms. Biomarker analyzes supported the diagnosis of Alzheimer’s disease in two patients with the diagnosis and suggested Alzheimer’s disease in another person; An autopsy analysis showed Alzheimer’s pathology in another patient.
The unusually young age at which these patients developed symptoms suggests that they did not have the usual sporadic Alzheimer’s that is associated with old age. In the five patients in whom samples were available for genetic testing, the team ruled out hereditary Alzheimer’s disease.
As treatment with c-hGH is no longer used, there is no risk of new transmission through this route . There have been no reported cases of Alzheimer’s acquired by any other medical or surgical procedure. There is no indication that beta-amyloid can be transmitted in everyday life or during routine medical or social care.
However, the researchers caution that their findings highlight the importance of reviewing measures to ensure there is no risk of accidental transmission of beta-amyloid through other medical or surgical procedures that have been implicated in the accidental transmission of Creutzfeldt disease. -Jakob (CJD).
Lead author of the research Professor John Collinge, director of the UCL Prion Diseases Institute and consultant neurologist at UCLH, said: "There is no suggestion that Alzheimer’s disease can be transmitted between individuals during family activities. daily life or routine medical activities. The patients we have described received a specific and long-discontinued medical treatment that consisted of being injected with material that is now known to be contaminated with proteins related to the disease .
“However, the recognition of the transmission of beta-amyloid pathology in these rare situations should lead us to review measures to prevent accidental transmission through other medical or surgical procedures, in order to prevent these types of cases from occurring.” in the future.
"Importantly, our findings also suggest that Alzheimer’s and some other neurological conditions share pathological processes similar to those of Creutzfeldt-Jakob disease (CJD), and this may have important implications for understanding and treating Alzheimer’s disease in the future. future".
Co-author Professor Jonathan Schott (UCL Queen Square Institute of Neurology, honorary consultant neurologist at UCLH and medical director of Alzheimer’s Research UK) said: "It is important to emphasize that the circumstances through which we believe these individuals developed Tragically, Alzheimer’s disease are highly unusual, and to reinforce that there is no risk that the disease can be transmitted between people or in routine medical care . However, these findings provide potentially valuable information about the mechanisms of the disease and pave the way for path for future research that we hope will improve our understanding of the causes of the most typical and late-onset Alzheimer’s disease.”
First author Dr Gargi Banerjee (UCL Institute of Prion Diseases) said: “We have discovered that it is possible for amyloid beta pathology to be transmitted and contribute to the development of Alzheimer’s disease. This transmission occurred after treatment with a now obsolete form of growth hormone and involved repeated treatments with contaminated material, often over several years. "There is no indication that Alzheimer’s disease can be acquired through close contact or during the provision of routine care."
The study was supported by the Medical Research Council, the National Institute for Health and Care Research (NIHR), the NIHR UCLH Biomedical Research Centre, Alzheimer’s Research UK and the Stroke Association.
Note : If you were treated with growth hormone (c-hGH) in the UK between 1959 and 1985 and would like more information about this research, please contact the National Prion Clinic by email (uclh.prion.help@nhs .net) or by phone (020 7679 5142 or 020 7679 5036)















