Instrumentation of the ear canal, foreign bodies, and slap or blast injuries are common causes of traumatic tympanic membrane perforations.
Tympanic membrane perforations ( TMP) usually present as sudden otalgia, hearing loss, and bloody otorrhea in the context of a causal mechanism.
Instrumentation of the ear canal accounts for approximately 60% of ear-related injuries (most commonly from cotton-tipped applicators). Diving or water sports are also well-recognized causes.
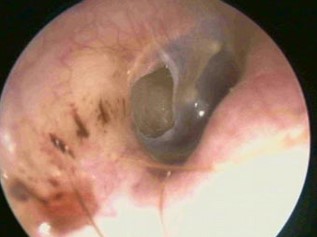
Perforations can be diagnosed solely with otoscopy findings .
Additionally, the absence of tympanic membrane mobility on pneumatic otoscopy or conductive hearing loss on tuning fork examination (tuning fork pressed on the forehead is heard louder in the affected ear) may help establish the diagnosis.
Audiometric testing is generally recommended 3 months after injury to confirm healing. In a study of 47 ears with traumatic conductive hearing loss, most audiogram results returned to normal with conservative treatment.
Patients should be advised to avoid getting water into the affected ear.
This can be accomplished by placing a cotton ball coated in Vaseline for showering or a silicone earplug for bathing or swimming.
The use of syringes for earwax extraction is contraindicated and should be discouraged as it can introduce infection.
Topical antibiotics (typically ciprofloxacin) are recommended if purulent otorrhea is present. Aminoglycosides should be avoided as they are ototoxic.
Most small traumatic perforations heal within 1 month.
A prospective study involving 126 patients with traumatic tympanic membrane perforations (TTM) showed that 72% of perforations smaller than a quarter of the size of the eardrum healed spontaneously within one month with conservative treatment, and only 25% of Larger perforations had closed at the same time.
Referral to otorhinolaryngology is indicated in cases of persistent or complicated traumatic perforations.
Patients with persistent tympanic membrane perforations (TMPs) 3 months after injury should be referred for surgical evaluation. Indications for otolaryngologic evaluation include retained foreign body, otorrhea refractory to 2 weeks of topical antibiotics, severe subjective hearing loss, tuning fork lateralizing to the unaffected ear (sensorineural hearing loss), vertigo or facial weakness (which may be indicative of an associated disease) injury to the inner ear).
References
↵Carniol ET, Bresler A, Shaigany K, et al. Traumatic tympanic membrane perforations diagnosed in emergency departments. JAMA Otolaryngol Head Neck Surg 2018;144:136–9.
↵Grant JR, Arganbright J, Friedland DR. Outcomes for conservative management of traumatic conductive hearing loss. Otol Neurotol 2008;29:344–9.
↵Rasool S, Ahmad F, Ahmad R. Traumatic tympanic membrane perforations: an overview in tertiary care hospital. Egypt J Otolaryngol 2016;32:187–90.
↵Harris AS, Elhassan HA, Flook EP. Why are ototopical aminoglycosides still first-line therapy for chronic suppurative otitis media? A systematic review and discussion of aminoglycosides versus quinolones. J Laryngol Otol 2016;130:2–7.
↵Lou ZC, Tang YM, Yang J. A prospective study evaluating spontaneous healing of aetiology, size and type-different groups of traumatic tympanic membrane perforation. Clin Otolaryngol 2011;36:450–60.