Out-of-hospital cardiac arrest (OHCA) is the leading cause of death in emergency room patients. Annually, more than 30,000 people in Korea suffer from OHCA and the survival rate is around 5%.
The low survival rate of OHCA could be due to progressive systemic injury in terms of aggravation of distal organ perfusion due to profound cardiogenic shock. In context, reducing distal organ nonperfusion is a critical point necessary to improve the survival rate of OHCA.
Recently, extracorporeal cardiopulmonary resuscitation has had improved clinical benefit for a patient who had fulminant myocarditis and acute myocardial infarction. Consequently, recent guidelines have recommended including consideration of extracorporeal cardiopulmonary resuscitation for selected patients with cardiac arrest.
Vitamin D is a well-known key factor in terms of calcium hemostasis, bone metabolism and modulation of the inflammatory process. Furthermore, vitamin D has a vital role in modulating the renin-angiotensin system and in the expression of genes related to myocardial hypertrophy.
Several investigations have addressed that vitamin D deficiency is a predisposing factor for cardiovascular morbidity and mortality, including myocardial dysfunction, hypertension, heart failure, and even sudden cardiac arrest (SCA).
A correlation between vitamin D levels and critically ill patients requiring extracorporeal membrane oxygenation (ECMO) has been reported. Furthermore, we have previously reported that vitamin D deficiency was associated with ACS and subsequent neurological outcome.
However, the association between OHCA with deep cardiogenic shock and vitamin D levels is unknown. This study aimed to investigate the association between vitamin D levels and deep cardiogenic shock in patients resuscitated from PCS.
Background:
Vitamin D deficiency is associated with various cardiovascular diseases, including sudden cardiac arrest (SCA). Profound cardiogenic shock is associated with morbidity and mortality in patients with PCS. This study investigated the association of vitamin D deficiency with profound cardiogenic shock in patients resuscitated from ACS.
Patients and methods:
We enrolled patients who were successfully resuscitated from out-of-hospital cardiac arrests for a presumed cardiac cause. Profound cardiogenic shock was defined as refractory hypotension requiring high-dose vasopressor infusion (norepinephrine > 0.5 mcg/kg/min) despite adequate intravascular volume replacement.
Vitamin D levels were measured as plasma 25(OH)D concentrations and severe vitamin D deficiency was defined as 25(OH)D <10 ng/ml.
Results:
A total of 237 subjects (179 men (76%), mean age 56.5 ± 16.5 years) were included in this study. The first monitored rhythm was shockable in 160 subjects (68%).
Mean arrest time and CPR times were 25.6 ± 15.7 and 22.8 ± 15.0 min, respectively. Profound cardiogenic shock was observed in 100 subjects (42%).
The mean vitamin D level was 12.3 ± 6.7 ng/ml and vitamin D deficiency was diagnosed in 109 subjects (46%).
In subjects with profound cardiogenic shock, vitamin D levels were significantly lower (10.7 ± 7.0 vs. 13.4 ± 6.2 ng/ml, P = 0.002) and severe vitamin D deficiency was observed more frequently (63% vs 34%, P < 0.001).
Subjects with profound cardiogenic shock are likely to have longer arrest times (29.5 ± 17.0 vs. 22.7 ± 14.0 min, P = 0.001), left ventricular systolic dysfunction (LVEF <40%, 73% vs. 38%, P <0.001), and baseline renal dysfunction (65% vs. 37%, P <0.001).
Multivariate logistic analysis indicated that vitamin D deficiency was significantly associated with profound cardiogenic shock after PCS (OR 2.71, 95% CI 1.42 to 5.18, P = 0.003) after adjusting for confounding variables.
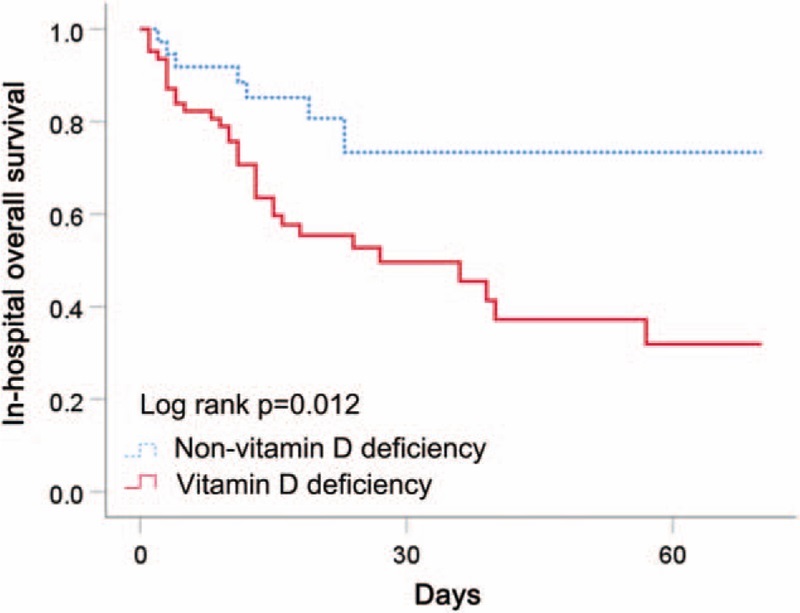
Survival curve of subjects with deep shock according to vitamin D deficiency.
Discussion
| The main findings of the present study are that deep cardiogenic shock in OHCA patients was highly prevalent and severe vitamin D deficiency had a strong correlation with deep cardiogenic shock and higher mortality rates in resuscitated OHCA patients. |
Profound cardiogenic shock is one of the significant poor prognostic factors in patients with OHCA. The cause of profound cardiogenic shock in patients with OHCA could be explained by the characteristics of postcardiac arrest syndrome (PCAS). Myocardial dysfunction following cardiac arrest, resulting in low cardiac output, hypotension, arrhythmia, and cardiovascular collapse, is one of the hallmarks of PCAS and contributes to the low survival rate in patients with cardiac arrest.
Similar to previous studies, our results revealed that patients with deep cardiogenic shock had a higher mortality rate and lower LVEF was a significantly associated variable for mortality in patients with deep cardiogenic shock.
Vitamin D has protective actions against cardiovascular diseases such as atherosclerosis, hypertension and heart failure. Vitamin D has a positive inotropic effect on cardiomyocytes. For example, vitamin D provides optimal myocardial contractility by regulating Ca2+ flux and sarcomere function and has a defensive role for cardiac hypertrophy by regulating physiological matrix turnover and cardiac remodeling.
Additionally, vitamin D acts as a downregulator of the renin-angiotensin system through vasodilatory secretion, adaptive arterial remodeling, and cardiac remodeling. Therefore, vitamin D deficiency suggests an unfavorable physiological effect on the function of the cardiovascular system.
Although post-cardiac arrest myocardial dysfunction in PCAS had poor clinical outcomes due to lack of distal organ perfusion, coronary blood flow is relatively preserved. Since coronary blood flow is preserved, LV systolic function can recover to the normal range after successful resuscitation.
Meanwhile, vitamin D plays a role in cardiac contractility to maintain optimal diastolic coronary perfusion. Recently, Sankar et al. reported that patients with vitamin D deficiency had a lower rate of shock reversal after OHCA with successful resuscitation.
Taken together, it could be suggested that vitamin D deficiency leads to insufficient diastolic coronary perfusion, which had poor clinical outcomes in OHCA patients with profound cardiogenic shock. In our results, patients with vitamin D deficiency had an association with deep cardiogenic shock and a higher mortality rate among patients with deep cardiogenic shock.
The present study had some limitations .
- First, it was a small, single-center study. Our results need to be confirmed in other multicenter trials.
- Second, baseline measured plasma 25(OH)D concentrations may not fully reflect a patient’s usual vitamin D status prior to OHCA.
- Third, although vitamin D deficiency remained an independent predictor of profound shock in sudden cardiac arrest and mortality, after adjusting for comorbidities and potential confounding variables, the possibility that severe deficiency cannot be ruled out. of vitamin D is only a risk marker, not a risk factor. Furthermore, statistical modeling may not fully correct for unmeasured confounding factors, including poor general health status, time of sunlight exposure, and adequate diet in the multivariate analysis.
Conclusions: Severe vitamin D deficiency was strongly associated with profound cardiogenic shock and mortality in patients resuscitated from PCS. |
















