Summary Hypertensive disorders of pregnancy (HDP) remain a leading cause of pregnancy-related maternal and fetal morbidity and mortality worldwide. Affected women also have an increased risk of cardiovascular disease later in life, independent of traditional cardiovascular disease risks. Despite the immediate and long-term cardiovascular disease risks, recommendations for the diagnosis and treatment of HDP in the United States have changed little or nothing in recent decades, unlike hypertension guidelines for the general population. The reasons for this approach include the question of the benefit of normalization of blood pressure treatment for pregnant women, together with theoretical concerns about fetal well-being from a reduction in utero-placental perfusion and in utero exposure to antihypertensive medication. This report is based on a review of the current literature and includes normal physiological changes in pregnancy that may affect the clinical presentation of HDP; epidemiology of HDP and the immediate and long-term sequelae of HDP; the pathophysiology of preeclampsia, a HDP commonly associated with proteinuria and increasingly recognized as a heterogeneous disease with different clinical phenotypes and probably different pathological mechanisms; a critical overview of current national and international HDP guidelines; Emerging evidence that lowering blood pressure treatment goals during pregnancy can reduce severe maternal hypertension without increasing the risk of pregnancy loss, high-level neonatal care, or overall maternal complications; and the increasingly recognized morbidity associated with postpartum hypertension/preeclampsia. Finally, we discuss the future of research in the field and the urgent need to study the socioeconomic and biological factors that may contribute to racial and ethnic disparities in maternal health care. |
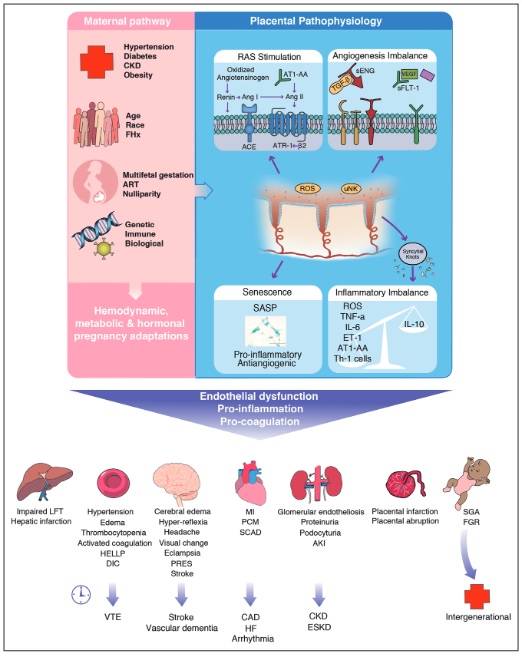
Pathogenesis of HDP: Pre-existing maternal comorbidities, non-modifiable patient characteristics, reproductive history, and genetic and immune factors increase the risk of developing hypertensive disorder of pregnancy (HDP). The molecular and pathophysiological mechanisms of preeclampsia are largely unknown, but the cause is likely to be a combination and interaction between factors from the maternal and placental pathways.61 The variable contributions of the underlying pathophysiological pathways of the mother and placenta result in the heterogeneous phenotypes of HDP. . The associated widespread endovascular damage and dysfunction may be long-lasting with a possible intergenerational effect.
Comments
Treatment for high blood pressure during pregnancy appears safe for many women and may reduce maternal risk of severe hypertension without increasing fetal and neonatal risks, according to a new scientific statement from the American Heart Association published in the journal Hypertension .
A scientific statement is an expert analysis of current research and can inform future clinical practice guidelines. In this statement, "Hypertension in Pregnancy: Diagnosis, Blood Pressure Goals, and Pharmacotherapy," experts in obstetrics and gynecology, maternal-fetal medicine, cardiology, nephrology, hypertension, and internal medicine reviewed and analyzed quality studies focused on blood pressure high during pregnancy including gestational hypertension and preeclampsia/eclampsia.
The latest statistics from the American Heart Association indicate that hypertension during pregnancy, defined as a systolic pressure of 140 mm Hg or higher , is the second leading cause of maternal death worldwide. Severe cases are associated with an increased risk of cardiovascular complications for mothers immediately or shortly after delivery and for years after pregnancy.
Hypertension during pregnancy increased the risks of complications for the offspring, such as preterm birth, small for gestational age, and low birth weight.
Rates of hypertension during pregnancy are increasing globally, and data indicate that it disproportionately affects women of diverse racial and ethnic backgrounds in the US, particularly those who are Black, American Indian, or Native American. Alaska.
The goals of treatment during pregnancy include preventing severe hypertension and preventing preterm birth to allow the fetus to mature before delivery.
“For decades, the benefits of blood pressure treatment for pregnant women were unclear. And there were concerns about fetal well-being due to exposure to antihypertensive medications,” said statement writing group chair Vesna D. Garovic, M.D., Ph.D., professor of medicine, chair of the division of nephrology and hypertension with a joint appointment in the department of obstetrics and gynecology at Mayo Clinic in Rochester, Minnesota.
“Through our comprehensive review of existing literature, it is reassuring to see emerging evidence that treating high blood pressure during pregnancy is safe and effective and may be beneficial at lower thresholds than previously thought. "Now, we have the current statement focused on hypertension during pregnancy to help inform optimal treatment and future research."
According to the statement, among high-income countries, the United States has one of the highest rates of maternal mortality related to hypertension. Cardiovascular diseases, including stroke and heart failure, now account for up to half of all maternal deaths in the US, and hospitalizations for pregnancy-related stroke increased more than 60% from 1994 to 2011.
Preeclampsia , which occurs when hypertension during pregnancy is accompanied by signs of liver or kidney problems such as protein in the urine, affects 5% to 7% of pregnancies and is responsible for more than 70,000 maternal deaths and 500,000 deaths . fetal deaths worldwide each year, according to the American Heart Association.
“Given the increasing number of cases of hypertension during pregnancy, along with complications related to hypertension, the problem has become a public health crisis, particularly among women of diverse ethnic and racial backgrounds,” Garovic said.
While the definition of hypertension for the general population is set at 130/80 mm Hg according to the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) Guidelines for Prevention, Detection, Evaluation, and Management For elevated blood pressure in adults, most guidelines worldwide define hypertension during pregnancy as 140/90 mm Hg .
There is a lack of consensus on when to start treatment for hypertension during pregnancy due to concerns about how the medications may affect the fetus. Several health advocacy groups recommend starting treatment when blood pressure measurements during pregnancy range between 140/90 mm Hg (Canadian guidelines) and 160/110 mm Hg (U.S. guidelines).
The new statement points to evidence that blood pressure-lowering therapy for hypertension of pregnancy significantly reduces the incidence of severe hypertension.
More research is needed to determine the extent to which treating hypertension at a lower threshold can decrease serious hypertensive complications, namely organ damage and hypertensive emergencies. Reducing severe hypertension may be particularly important in communities that lack resources and expertise to respond to hypertension emergencies, the statement’s authors write.
“Future studies should address whether lowering the threshold for hypertension treatment during pregnancy could allow for safe and timely blood pressure control and avoid hasty delivery due to uncontrolled hypertension,” Garovic said.
So far, the latest research indicates that treating hypertension during pregnancy with blood pressure-lowering medications does not appear to have a negative impact on fetal growth or development. Preventing hypertension during pregnancy promotes maternal health both during and after pregnancy .
It is well known that those who have hypertension during pregnancy are more likely to develop sustained hypertension after pregnancy at a higher rate compared to those whose blood pressure was normal during pregnancy. The statement reinforces recent research suggesting that lifestyle changes before and during pregnancy have the potential to improve maternal and fetal outcomes:
- Dietary changes before and during pregnancy can limit weight gain and improve pregnancy outcomes.
- Exercise during pregnancy can reduce the risk of gestational hypertension by about 30% and the risk of preeclampsia by about 40%.
The statement also highlights these areas of concern:
- There is emerging evidence that hypertension after childbirth (postpartum) may be associated with important maternal health problems.
- Current science suggests that physicians should individualize treatment decisions, considering risk factors and patient preferences.
- The care of women with hypertension during pregnancy is often complex and a multispecialty team of health professionals may be beneficial.
"Future clinical trials are needed to address questions about when to start treatment for high blood pressure during pregnancy," Garovic said. "In addition, close collaboration between the American Heart Association and the American College of Obstetricians and Gynecologists will be critical to optimizing the diagnosis and treatment of hypertension during pregnancy and to improving immediate and long-term outcomes for many women who develop hypertension During pregnancy".
This scientific statement was prepared by the group of volunteer writers on behalf of the Hypertension Council of the American Heart Association; the Scientific Subcommittee of the Council on the Kidney in Cardiovascular Diseases; the Council on Atherosclerosis, Thrombosis and Vascular Biology; the Cardiometabolic Health and Lifestyle Council; the Council on Peripheral Vascular Diseases; and the Stroke Council.
Access the full text in English
The American Heart Association’s scientific statements promote greater awareness of cardiovascular disease and stroke problems and help facilitate informed health care decisions. Scientific statements describe what is currently known about a topic and what areas need additional research. While scientific statements inform guideline development, they do not make treatment recommendations. The American Heart Association guidelines provide the Association’s official clinical practice recommendations.
Co-authors are Vice President Phyllis August, MD, MPH.; Ralf Dechend, M.D.; S. Ananth Karumanchi, MD.; Suzanne McMurtry Baird, DNP, RN.; Thomas Easterling, M.D.; Laura A. Magee, MD.; Sarosh Rana, MD, MPH.; and Jane V. Vermunt, MBCh.B., M.Sc. Author disclosures are listed in the manuscript.
















