Background
Clinical risk factors, a single blood pressure (BP) measurement, current biomarkers, and biophysical parameters can effectively identify the risk of early-onset preeclampsia , but have limited ability to predict late-onset preeclampsia and hypertension. gestational. Clinical BP patterns hold promise for improving early risk stratification of hypertensive disorders of pregnancy.
Methods and Results
After excluding preexisting hypertension, heart, kidney, or liver disease, or prior preeclampsia, the retrospective cohort (n=249,892) had systolic BP <140 mm Hg and diastolic BP <90 mm Hg or a single BP elevation ≤20 weeks of gestation, prenatal care at <14 weeks’ gestation, and delivery of a live or stillborn newborn at Kaiser Permanente hospitals in Northern California (2009–2019).
The sample was randomly divided into development (N=174,925; 70%) and validation (n=74,967; 30%) data sets.
The predictive performance of multinomial logistic regression models for early-onset preeclampsia (<34 weeks), late-onset preeclampsia (≥34 weeks), and gestational hypertension was evaluated in the validation data set. There were 1008 (0.4%), 10,766 (4.3%), and 11,514 (4.6%) patients with early-onset preeclampsia, late-onset preeclampsia, and gestational hypertension, respectively.
Models with 6 systolic BP trajectory groups (0-20 weeks gestation) plus standard clinical risk factors performed substantially better than risk factors alone in predicting early- and late-onset preeclampsia and gestational hypertension, with statistical C (95% CI) of 0.747 (0.720–0.775), 0.730 (0.722–0.739), and 0.768 (0.761–0.776) vs. 0.688 (0.659–0.717), 0.695 (0.686–0.704), and 0.692 (0.683–0.7 01) , respectively, with excellent calibration (Hosmer ‐Lemeshow P=0.99, 0.99 and 0.74, respectively).
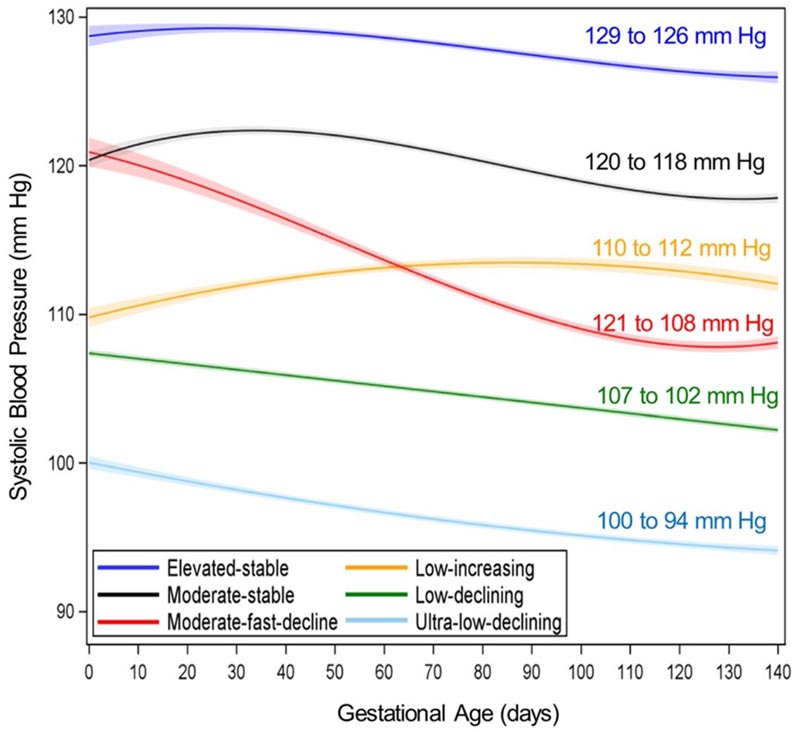
Figure . Six early pregnancy systolic blood pressure (BPT) trajectory groups from 0 to 20 weeks gestation (from baseline to last measurement of average blood pressure in mm Hg for each BPT group ).
Six groups of BPT in early pregnancy: ultra-low decrease (light blue), low decrease (green), moderate to rapid decrease (red), low increase (yellow), moderate stable (black) and high stable (purple). Adapted from Gunderson et al10 with permission. Copyright ©2022 Wolters Kluwer Health, Inc.
Conclusions BP patterns from early pregnancy to 20 weeks’ gestation plus clinical, social, and behavioral factors more accurately discriminate risk hypertensive disorders among low- to moderate-risk pregnancies. Early BP trajectories in pregnancy improve risk stratification to reveal higher-risk individuals hidden within ostensibly low-to-moderate risk groups and lower-risk individuals considered higher risk according to Preventive Services Task Force criteria. from USA |
Clinical Perspective
What are the clinical implications?
Classification of early pregnancy systolic BP patterns based on BP changes from 0 to 16 to 20 weeks’ gestation in combination with other standard risk factors (clinical, social, and behavioral) may significantly improve individual risk stratification. for early- and late-onset preeclampsia and gestational hypertension, allowing for more targeted surveillance and potentially interventions to improve hypertensive disorders of pregnancy and adverse outcomes, as well as avoiding additional monitoring or unnecessary interventions (i.e., administration of low-dose aspirin) in low-risk pregnancies.
In the future, these findings may be translated into an automated clinical tool within the electronic health records system, or a web-based tool to classify changes in BP pattern during early gestation for individual risk stratification of preeclampsia. or gestational hypertension that can improve precision medicine by more accurately identifying patients who can truly benefit most from better monitoring and intervention(s).
















