Summary Background Among women with hypertensive disorders of pregnancy, biomarkers can stratify the risk of developing preeclampsia with severe features (sPE). Methods At 18 US centers, we prospectively measured the relationship between serum soluble fms-like tyrosine kinase 1 (sFlt-1) and placental growth factor (PlGF) in pregnant women hospitalized between 23 and 35 weeks of gestation. The primary outcome was prediction of sPE and secondary outcomes included prediction of adverse outcomes within 2 weeks. The prognostic performance of the sFlt-1:PlGF ratio was evaluated using a derivation/validation design. Results A total of 1014 pregnant women were evaluated ; 299 were included in the derivation cohort and 715 in the validation cohort. In the derivation cohort, the median sFlt-1:PlGF ratio was 200 (interquartile range, 53 to 458) among women who developed sPE compared with 6 (interquartile range, 3 to 26) in those who did not. (P < 0.001). The discriminatory ratio of ≥40 was then tested in the validation cohort and yielded a positive predictive value of 65% (95% confidence interval [CI], 59 to 71) and negative predictive value of 96% (95% CI, 93 to 98) for the primary outcome. The ratio performed better than standard clinical measures (area under the receiver operating characteristic curve, 0.92 versus <0.75 for standard-of-care tests). Compared with women with a ratio <40, women with a ratio ≥40 had a higher risk of adverse maternal outcomes (16.1% vs. 2.8%; relative risk, 5.8; 95% CI). 2.8 to 12.2). Conclusions In women with a hypertensive disorder of pregnancy presenting between 23 and 35 weeks of gestation, measurement of serum sFlt-1:PlGF provided risk stratification of progressing to sPE within the next two weeks. |
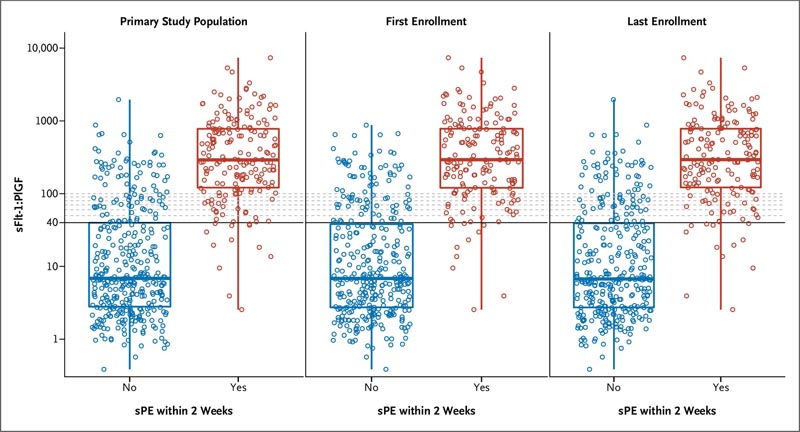
Figure 1. Serum sFlt-1:PlGF ratio in women who do or do not develop sPE over 2 weeks. Distributions of soluble fms-like tyrosine kinase 1 (sFlt-1):placental growth factor (PlGF) ratios (vertical axis on log scale) in strata according to preeclampsia with severe features (sPE) within 2 weeks (horizontal axes, enrollments that developed sPE in red, preeclampsia without severe features in blue for the primary study population and when counting only the first or last enrollment). The box represents the median with the interquartile range (25th to 75th percentiles), and the whiskers represent the minimum and maximum values.
Comments
In a study of pregnant women in the United States, Cedars-Sinai researchers found that a specific imbalance of two placental proteins could predict which women were at risk of developing a severe form of preeclampsia, a potentially fatal blood pressure disorder.
The study is published in the journal NEJM Evidence .
"We found that a blood test that measures the ratio between two proteins involved in the development of blood vessels in the placenta could identify which women would develop premature preeclampsia with severe features," said study co-senior author Sarah Kilpatrick, MD, PhD, chair of the Department of Obstetrics and Gynecology at Cedars-Sinai. “This test was significantly better than all standard-of-care markers for preeclampsia with severe features. “It predicted with more than 90% accuracy whether the patient would develop preeclampsia with severe features or not, while the usual markers were accurate less than 75% of the time.”
The prospective, blinded study of women initially hospitalized for premature hypertension involved 1,014 patients from 18 hospitals nationwide.
“This multicenter investigation is one of the few large studies of the risk of developing preeclampsia with severe features in the US. The women represented a more racially diverse cohort than previous studies and included patients from smaller community hospitals and large academic medical centers. , in both cities and rural areas,” Kilpatrick said.
Preeclampsia is the most common hypertensive disorder associated with pregnancy. The severe form of the disease can cause dangerously high blood pressure, organ failure, vision loss or even a stroke. It affects approximately 5% of pregnant women and is a leading cause of maternal and fetal death and serious illness.
Researchers found that a specific protein imbalance revealed in blood tests of hospitalized pregnant women provided a way to quantify their risk of developing severe preeclampsia. It involves levels of soluble fms-like tyrosine kinase 1 (sFlt-1) and placental growth factor (PIGF) in the bloodstream.
"An sFlt-1 to PIGF ratio of 40 or greater predicted the development of severe preeclampsia, adverse outcomes, and preterm birth within two weeks, two-thirds of the time," said S. Ananth Karumanchi, MD, co-senior author of the study, who is the Medallion Chair in Vascular Biology.
"In contrast, if the critical ratio between the two proteins was below 40, we found that the risk of the patient progressing to preeclampsia with severe features within two weeks after the blood test was less than 5%," said Karumanchi, who is also director of Nephrology at Cedars-Sinai.
Currently, the only cure for preeclampsia is childbirth. A test indicating that a premature patient, a woman who has completed less than 37 weeks of pregnancy, is likely to develop serious illness could help optimize care.
“We anticipate that this blood test may eventually lead to better health outcomes for mothers and their babies,” Kilpatrick said. “It is well known that preeclampsia progresses in virtually all patients until they give birth. But it can be very difficult to predict the optimal time for delivery. Having an accurate test would help us ensure that the mother was in the appropriate hospital for the management of her care and that of her premature baby.”
Preeclampsia rates have been steadily increasing, largely due to rising obesity and hypertension in the country. Black, American Indian, and Alaska Native women have significantly higher rates of disease than white women and a higher risk of death.
The researchers also hope that the findings can point the way toward possible drug therapies for women at risk.
"We know that sFlt-1 is the protein that increases even before any symptoms of preeclampsia occur and the ratio of sFlt-1 to PlGF predicts worsening of the disease," Karumanchi said. “Further research may identify a pharmacological mechanism that could reduce sFlt-1 levels and be used to safely prolong pregnancy; “That would be a game changer for patients with very premature preeclampsia.”
While the study involved a single blood test of two proteins, researchers are encouraged that more research, involving large numbers of subjects, will provide better tools to thwart preeclampsia before it can seriously harm patients and their babies.
"We conducted this study to identify a simple and accurate biomarker that doctors can use to determine who is at highest risk for preeclampsia with severe features and who would be a suitable candidate for treatments we could develop for this devastating condition," said the study’s co-author. . senior author Ravi Thadhani, MD, MPH, professor of medicine at Harvard Medical School, chief academic officer at Mass General Brigham, in Boston, Massachusetts, and visiting faculty scientist at Cedars-Sinai. "I believe we achieved this goal."
In summary , in a demographically diverse cohort of pregnant women with hypertension in the United States hospitalized between 23 and 35 weeks of gestation, serum sFlt-1:PlGF ratio of 40 predicted the development of sPE, adverse outcomes, and delivery within 2 weeks after the test.
Funding: Cedars-Sinai and Thermo Fisher Scientific provided support for the study.
















