"Depression is a mood disorder, so mysteriously painful and elusive in the way it becomes known to the self, to the mediating intellect, that it is almost beyond description. Therefore, it remains almost incomprehensible for those who have not experienced it in its extreme mode.” William Styron (Darkness Visible, 1990)"
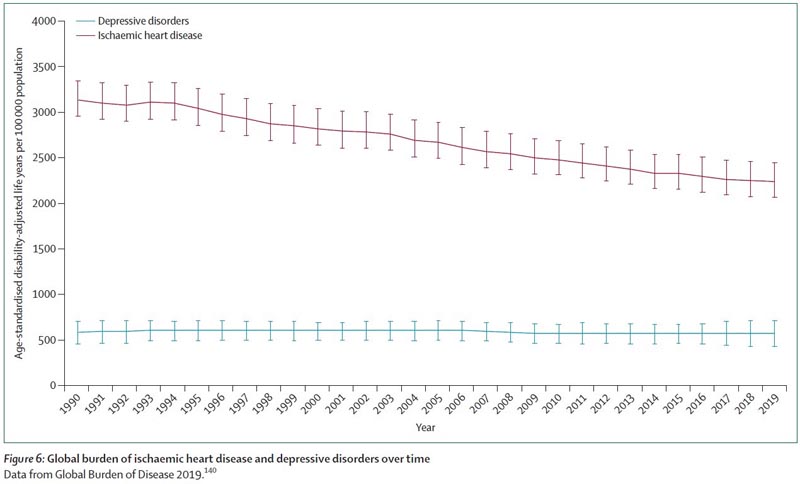
Evidence has been accumulating for decades that depression is one of the leading causes of preventable suffering in the world. However, very few people in communities, governments and the health sector understand or recognize depression as distinct from other problems people face. Not enough is being done to prevent and alleviate the suffering and disadvantage related to depression, and few governments recognize the brakes that depression places on economic and social development.
Data
|
Key messages
1 Depression is a common but poorly recognized and understood health condition
Depression can cause profound distress, impair social functioning and economic productivity, and lead to premature mortality; It has substantial impacts on families and society. However, these impacts are not well understood or recognized, and there is an insufficient response at local and international levels. Many factors related to the prevention and treatment of depression remain unknown, such as what works for whom and why, and more scientific discoveries are required, as well as better implementation of current management strategies to transform the lives of people. millions of people and their families and communities facing these challenges.
2 Depression is a heterogeneous condition
This term encompasses depressive disorders, as well as symptoms of depression that cause distress or social impairment; The depression experienced by people diagnosed with bipolar disorder is outside the scope of the Commission.
Although generally classified as a binary disorder, depression has a diversity of clinical presentations, levels of severity, and longitudinal courses; It extends beyond the limits imposed by current classifications and commonly overlaps with other conditions.
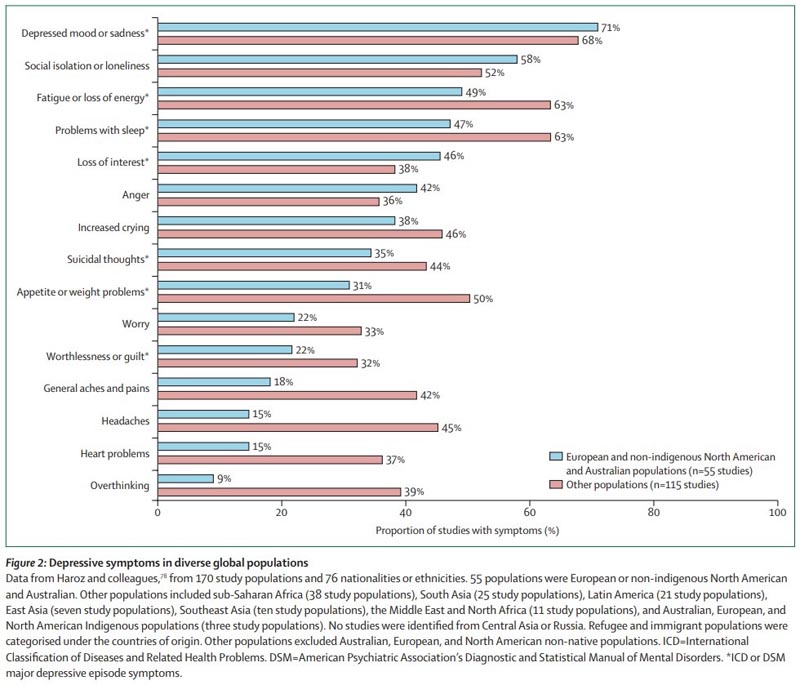
3 Depression is universal, but culture and context matter
Depression has been described throughout the eons of human civilization. Depressed mood, loss of interest, and fatigue are common features of the condition across populations. However, there is also considerable variability in the types and prevalence of depressive symptoms and signs across cultures and contexts.
4 Prevention is essential to reduce the burden of depression globally
Social and economic actions are needed throughout society to mitigate the effects of adversities and inequalities in early life and throughout the life course. Interventions are also needed at the individual level, focusing on current lifestyle habits and risk factors. More efficient depression prevention is likely to have a major impact on a country’s Sustainable Development Goals and the health of individuals and families.
5 The experiences of depression and recovery are unique to each individual
Depression is the result of a set of factors, typically the interaction of proximal adversities with genetic, social, environmental, and developmental risk and resilience factors. There is a frequent and complex association between depression and physical health. No two people share the same life history and constitution, which ultimately leads to a particular experience of depression and different requirements for help, support and treatment in recovery.
6 Closing the care gap requires the participation of people with lived experience
Most people with depression around the world do not receive effective care due to a variety of supply and demand barriers. It is vital to empower individuals, families and communities to work with professionals who can learn from their experiences and help demand the implementation of known preventive and therapeutic strategies and hold healthcare systems and decision makers accountable. .
7 A formulation is needed to personalize care
Detection and diagnosis of depression on the basis of symptoms, function and duration must be accompanied by a clinical review or formulation for each person, taking into account individual values and preferences, life histories and circumstances. . The formulation identifies characteristics that favor personalized treatment. The complexity and sophistication of the formulation may vary depending on the context of care and the availability of resources.
8 A staged care approach addresses the heterogeneous nature of depression and its impacts on individual, family, and community functioning
A staged approach offers a pragmatic tool to translate the heterogeneous clinical nature of depression for management and ensure that interventions are comprehensive but proportional to the severity of the condition. This approach facilitates a focus on intervention early in the course of the condition and grading the intensity of interventions, tailored to the specific needs of the person and stage of the disease.
9 Collaborative delivery models are a cost-effective strategy for scaling depression interventions into routine care.
10 Greater investment with participation of the whole society is a priority to translate current knowledge into practice and policy and to update the scientific agenda
Although much is still unknown about depression, for which we advocate for a cutting-edge scientific agenda, current knowledge and strategies are not optimally used; The most important immediate imperative is to invest in the translation of this rich body of knowledge into practice and policy.
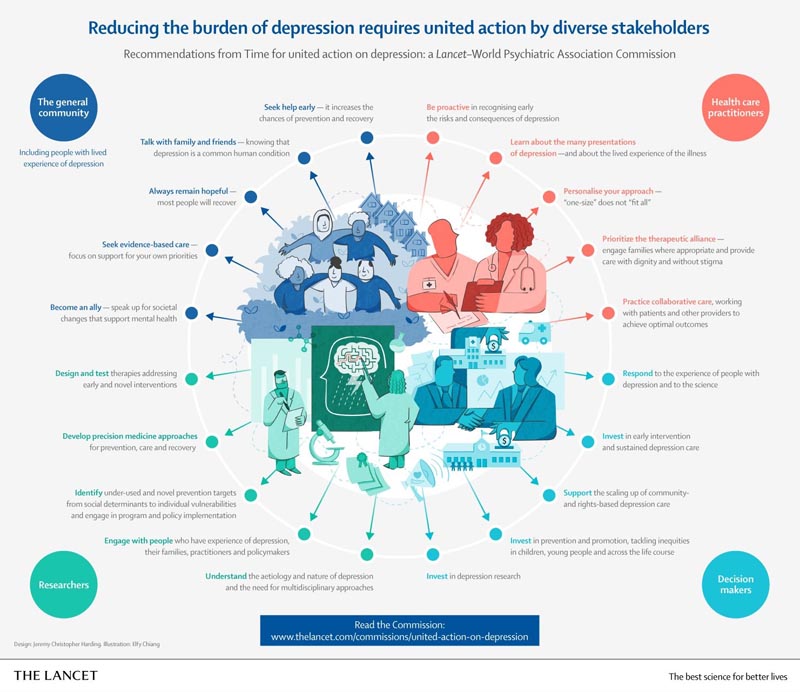
- The Commission calls for a whole-of-society approach to alleviate one of the world’s leading causes of avoidable suffering and premature death.
- Myth: Depression is simply sadness. Each year, approximately 5% of adults live with this distinct health condition. But much can be done to prevent #depression and help recovery.
- With or without clinical depression: the current system of classifying people with symptoms is too simplistic .
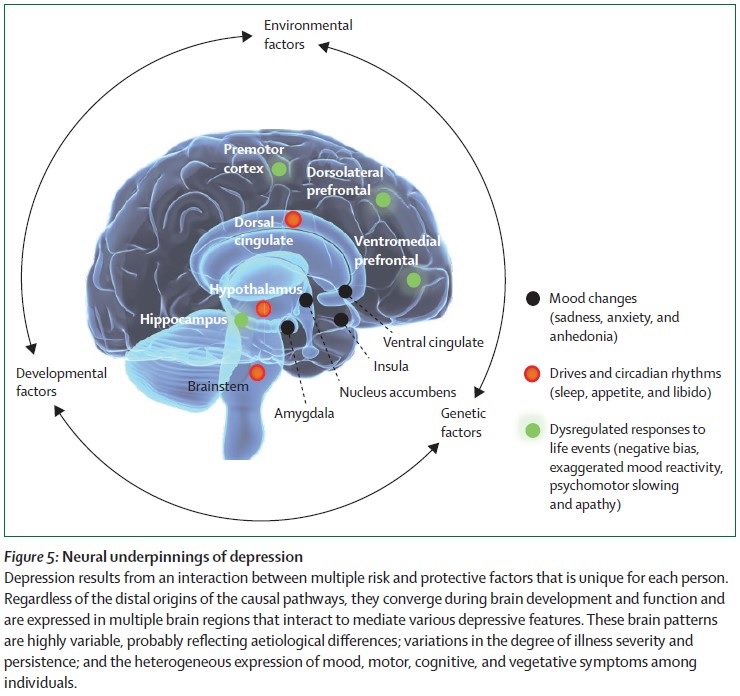
- Depression is complex and a personalized, staged approach to care is vital to reducing the overall burden. Most research on depression comes from mainly English-speaking HICs. The core characteristics of depression can be identified across cultures and regions, but its essential variations are recognized.
- There is no reduction in the global impact of #depression in the last 3 decades, estimates suggest. Comparison with coronary artery disease.
Comments
Collaborative care offers an evidence-based approach to the delivery of interventions by diverse providers, tailored to the specific stage of the disease and always including participatory decision making with patients and engagement with families and communities , which greatly increases the possibilities for rights-based quality. care and referral and recovery.
The world is failing to address the persistent and worsening global depression crisis it faces, according to The Lancet Commission on Depression and the World Psychiatric Association, calling for a whole-of-society response to reduce the burden depression world.
Despite abundant evidence that much can be done to prevent depression and aid recovery even in resource-limited settings, an estimated 5% of the world’s adult population in any year lives with depression.
In high-income countries, approximately half of people suffering from depression are undiagnosed and untreated, and this rises to 80-90% in low- and middle-income countries. The COVID-19 pandemic has created additional challenges, as social isolation, grief, uncertainty, hardship and limited access to healthcare are severely impacting the mental health of millions of people.
In this context, the ’It’s Time for United Action Against Depression’ Commission calls for concerted and collaborative efforts by governments, healthcare providers, researchers, people living with depression and their families to improve care and prevention, fill knowledge gaps and raise awareness to address one of the leading causes of preventable suffering and premature death around the world. It is written by 25 experts from 11 countries spanning disciplines from neuroscience to global health and is advised by people with experience in depression.
“Depression is a global health crisis that requires responses at multiple levels. This Commission offers an important opportunity for united action to transform approaches to mental health care and prevention globally. Investing in reducing the burden of depression will give millions of people the opportunity to become healthier, happier and more productive members of society, help strengthen national economies and advance the United Nations Sustainable Development Goals for 2030 ” says Commission Chair Professor Helen Herrman of Orygen, National Center for Excellence in Youth Mental Health and the University of Melbourne, Australia.
Co-author Dr Charles Reynolds from the University of Pittsburgh, USA, says: “We know that most people with depression at all stages of life will recover if they get the right support and treatment. With sound science, political will, and shared responsibility, depression can be prevented and treated and its potentially disabling consequences avoided. We must empower people with experience of depression together with families, doctors, policymakers and civil society to address the tsunami of unmet needs, sharing their experiences to reduce stigma, supporting others with information about the condition and possibilities for help, and advocating for increased resources for evidence-based approaches.”
A poorly recognized and understood condition
Depression is a common condition throughout the world, however, despite this, many myths continue to surround it, perpetuating inaction. These include common misconceptions that depression is simply sadness, a sign of weakness, or is restricted to certain cultural groups.
The Commissioners emphasize that depression is a distinct health condition characterized by its persistence, substantial effect on daily functioning, and long-term health consequences. It can affect anyone, regardless of sex, origin, social class or age. There is variability in the types and prevalence of depressive symptoms and signs across cultures and populations. The risk of depression increases in environments of adversity, such as poverty, violence, displacement, and gender, racial and other forms of discrimination.
Depression is linked to a wide variety of chronic physical illnesses, and a person’s physical health can influence their mental health, and vice versa.
In the worst case, depression can lead to suicide. Studies indicate that between 70% and 80% of people who die by suicide in high-income countries, and about half of people in low- and middle-income countries, suffer from mental illnesses, including depression. It is the most common cause.
Depression also has an enormous and underrecognized social and economic cost on individuals, families, communities and countries. Even before the COVID-19 pandemic, the loss of economic productivity linked to the depression cost the global economy an estimated US$1 trillion annually.
“There is possibly no other health condition that is as common, as burdensome, as universal or as treatable as depression, but receives little political attention and resources,” says Commission co-chair Associate Professor Christian Kieling of the Universidade Federal do Rio. Grande do Sul in Brazil. “Effective psychosocial and medical treatments are difficult to access, while high levels of stigma still prevent many people, including the high proportion of adolescents and young people at risk of or suffering from depression, from seeking the help they need to lead a healthy life.” and productive.”
Prevention is essential to reduce the burden of depression
The Commission emphasizes the need for society-wide strategies that reduce exposure to both adverse experiences in childhood (including neglect and trauma) and across the lifespan to reduce the prevalence of depression. Interventions are also needed at the individual level, focusing on lifestyle factors (e.g., smoking, alcohol use, physical inactivity) and other risk factors, such as intimate partner violence and stressful life events such as grief. or the financial crisis.
“Prevention is the most neglected aspect of depression. This is partly because most interventions are outside the health sector ,” says co-author Dr. Lakshmi Vijayakumar of SNEHA, Suicide Prevention Center and Voluntary Health Services, Chennai, India. “In the face of the lifelong effects of teenage depression, from difficulties in school and future relationships to the risk of substance abuse, self-harm and suicide, investing in depression prevention is an excellent value for money. It is crucial that we implement evidence-based interventions that support parenting, reduce family violence and bullying, as well as promote mental health at work and address loneliness in older adults. “Common risk factors and high rates of depression among people with chronic health problems also support shared preventive approaches.”
A personalized, staged approach to care
The commissioners emphasize that the current system of classifying people with symptoms of depression into just two categories, whether they have clinical depression or not, is overly simplistic. They argue that depression is a complex condition with a diversity of signs and symptoms, levels of severity and duration across cultures and the life course.
The Commission supports a personalized and staged approach to depression care that recognizes the timing and intensity of symptoms and recommends interventions tailored to the individual’s specific needs and severity of the condition, ranging from self-help and changes in lifestyle to psychological therapies and antidepressants to more intensive and specialized treatments, such as electroconvulsive therapy (ECT) for severe and refractory forms of the disease.
“No two people share the exact life history and constitution, which ultimately leads to a unique experience of depression and different needs for help, support and treatment,” explains Professor Vikram Patel, co-chair of the Commission, from Harvard Medical School in the US. “Similar to cancer care, the staged approach looks at depression along a continuum, from well-being to temporary distress to an actual depressive disorder, and “It provides a framework for recommending proportional interventions from the earliest point of the disease.”
At the same time, the Commission proposes that collaborative care strategies be adopted to scale up evidence-based interventions in routine care.
They argue that the use of locally recruited, widely available, low-cost non-specialists such as community health workers and lay counselors not only addresses the serious shortage of qualified providers and financial barriers, but will also help reduce stigma and cultural barriers, while providing comprehensive care to patients and their families. While this is most important in low-income countries, it is also universally relevant and useful, as nowhere in the world is depression care adequate.
Ultimately, greater investment is needed to ensure that people receive the care they need where and when they need it, and the Commission underscores the importance of whole-of-government action to reduce the harmful effects of poverty, inequality of gender and other social inequities on mental health.
“Policies that reduce racial or ethnic inequalities, the systematic disadvantages experienced by women, and support fair income distribution through universal health coverage and expanding opportunities for educational attainment can be potentially powerful preventive strategies.” says Herrman. “Addressing the climate emergency, the COVID-19 pandemic and other global and regional emergencies that exacerbate existing inequalities and threats to health, including the pursuit of the UN Sustainable Development Goals, must also be vital parts of efforts to prevent depression.
















