Key points What is the dynamic trajectory of cognitive changes in the elderly population surviving COVID-19? Findings In this cohort study of 1,438 COVID-19 survivors aged 60 years or older who were discharged from COVID-19-designated hospitals in Wuhan, China, the incidence of cognitive impairment was higher in COVID-19 survivors, especially in those with severe cases, compared to uninfected participants over a 1-year follow-up period. Meaning The findings suggest that long-term cognitive impairment is common after SARS-CoV-2 infection, indicating the need to evaluate the impact of the COVID-19 pandemic on the future burden of dementia worldwide. |
Introduction
The COVID-19 pandemic has affected more than 418 million patients so far, and the number is increasing. The long-term impact of COVID-19 on cognition has become a major public health issue.
SARS-CoV-2 causes a variety of neurological sequelae in COVID-19 survivors, including dizziness, headache, myalgia, hypogeusia, hyposmia, polyneuropathy, myositis, cerebrovascular diseases, encephalitis, and encephalopathy. Such susceptibility of the central nervous system to SARS-CoV-2 has sparked great interest in neuropsychiatric research among COVID-19 survivors.
Cognitive complaints are common in the acute and subacute phases of COVID-19. Our research, along with that of others, has demonstrated an association between SARS-CoV-2 infection and cognitive performance in older adults months after infection. However, the long-term trajectory of cognitive changes after SARS-CoV-2 infection remains unknown. In this study, we investigated the 1-year dynamic trajectory of cognitive changes in older COVID-19 survivors.
Importance
Determining the long-term impact of COVID-19 on cognition is important to inform immediate steps in COVID-19 research and health policy.
Aim
To investigate the 1-year trajectory of cognitive changes in older COVID-19 survivors.
Design, environment and participants
This cohort study recruited 3,233 COVID-19 survivors aged 60 years or older who were discharged from 3 designated COVID-19 hospitals in Wuhan, China, from February 10 to April 10, 2020.
Their uninfected spouses (N = 466) were recruited as a control population. Participants with cognitive impairment prior to infection, a concomitant neurological disorder, or a family history of dementia were excluded, as were those with severe heart, liver, or kidney disease or any type of tumor.
Follow-up of cognitive functioning and impairment was performed at 6 and 12 months. A total of 1438 COVID-19 survivors and 438 control individuals were included in the final follow-up. COVID-19 was classified as severe or non-severe following American Thoracic Society guidelines.
Main results and measures
The primary outcome was change in cognition 1 year after patient discharge. Cognitive changes during the first and second 6-month follow-up periods were assessed using the Informant Questionnaire on Cognitive Decline in the Elderly and the Telephone Interview on Cognitive Status, respectively.
Based on the cognitive changes observed during the 2 periods, the cognitive trajectories were classified into 4 categories:
- Stable cognition.
- Early onset cognitive impairment.
- Late-onset cognitive impairment.
- Progressive cognitive impairment.
Conditional and multinomial logistic regression models were used to identify factors associated with the risk of cognitive decline.
Results
Among the 3,233 COVID-19 survivors and 1,317 uninfected spouses examined, 1,438 participants who were treated for COVID-19 (691 men [48.05%] and 747 women [51.95%]; median [IQR] age , 69 [66-74] years) and 438 uninfected control individuals (222 men [50.68%] and 216 women [49.32%]; median [IQR] age, 67 [66-74] years) completed the 12-month follow-up.
The incidence of cognitive impairment in survivors 12 months after discharge was 12.45%. Individuals with severe cases had lower scores on the Cognitive Status Telephone Interview-40 than those with non-severe cases and control individuals at 12 months (median [IQR]: severe, 22.50 [16.00-28.00]; non-severe, 30.00 [26.00-33.00]; control, 31.00 [26.00-33.00]). Severe COVID-19 was associated with an increased risk of early-onset cognitive decline (odds ratio [OR], 4.87; 95% CI, 3.30-7.20).
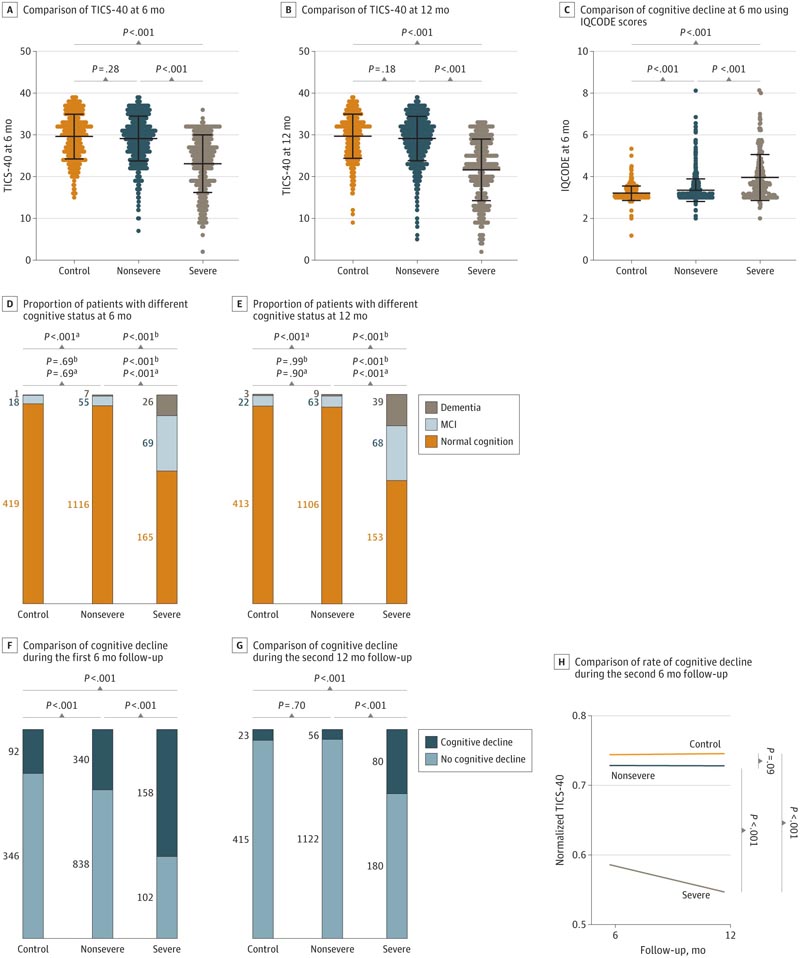
Comparison of Telephone Interview of Cognitive Status-40 (TICS-40) scores between severe COVID-19 survivors, non-severe COVID-19 survivors, and uninfected control individuals at 6 and 12 months was calculated using Wilcoxon test (Mann-Whitney U). The proportions of participants with different cognitive states at 6 and 12 months were calculated using the χ 2 test. Informant Questionnaire on Cognitive Impairment in the Elderly (IQCODE) scores ≥3.5 were considered indicative of cognitive impairment. A decrease of ≥3 points on the TICS-40 from baseline during follow-up was considered indicative of clinically significant cognitive impairment. H, Values adjusted for age, sex, education, body mass index and each comorbidity using linear mixed effects models. Data normalization was performed using min-max normalization.
a Difference in mild cognitive impairment.
b Difference in dementia.
Discussion
Postinfection cognitive outcomes following COVID-19 have been reported, but the long-term dynamic trajectory of cognitive changes in COVID-19 survivors remains unclear. Previous pandemics have provided evidence showing the adverse effects of severe respiratory diseases on cognitive functions.
Approximately 15% of patients infected with severe acute respiratory syndrome or Middle East respiratory syndrome showed long-term cognitive deficits, such as memory and attention problems. 22 With the increasing number of patients surviving COVID-19, the cognitive sequelae of this disease have attracted much attention.
Recent studies found that COVID-19 was associated with an increased risk of being diagnosed with dementia within 6 months of infection. Consistent with this, we found that approximately 3.3% of COVID-19 survivors had dementia and 9.1% had MCI at 12 months after discharge; In particular, the incidences of dementia and MCI were 15.00% and 26.15% in individuals with severe cases, respectively.
The incidence of dementia or mild cognitive impairment was not different between individuals with nonsevere cases and uninfected control individuals. These findings suggest that COVID-19, especially severe COVID-19, may be associated with long-term cognitive impairment.
Conclusions and relevance In this cohort study of COVID-19 survivors aged 60 years or older who were discharged from COVID-19-designated hospitals in Wuhan, China, SARS-CoV-2 infection, especially severe infection, was associated with an increased risk of longitudinal cognitive decline. The results highlight the importance of immediate measures to address this challenge. |