In the era of collective decline in cancer incidence, the incidence of anal, oropharyngeal, and vulvar cancer associated with human papillomavirus (HPV) is increasing rapidly , while the incidence of cervical cancer has stabilized in the recent years in the United States.
Risk factors for HPV-associated cancers (e.g., current smoking, risky sexual behaviors) are more common in poorer counties. Therefore, trends in HPV-associated cancer incidence in low-income counties and those with high smoking prevalence may differ from their counterparts, but are not described.
Understanding calendar trends in the incidence of HPV-associated cancers by these attributes at the county level may help disentangle disparities and inform targeted prevention interventions.
During 2000-2018, higher incidence rates of HPV-associated cancers were observed in counties with the lowest household income and highest prevalence of smoking. Additionally, disparities in the incidence of HPV-associated anal, oropharyngeal, and vulvar cancer increased between low- and high-income counties and those with the highest prevalence of smoking compared to their counterparts.
Summary The burden of cancer associated with human papillomavirus (HPV) is increasing in the United States. Trends in county-level income incidence and smoking prevalence remain undescribed. We used the Surveillance, Epidemiology, and End Results 21 database to determine HPV-associated cancers during 2000-2018. Trends were estimated by county-level income and smoking prevalence quartiles. Anal and vulvar cancer incidence among women and anal cancer incidence among men increased markedly in lower-income counties, while increases were slower in higher-income counties (p. range [CI ] = 0.9% to 2.9%, in lower-income counties vs. 0.8% per year, 95% CI = 0.6% to 1.1%, in higher-income counties ). In recent years, cervical cancer incidence has stabilized (0.0% per year [95% CI = -0.5% to 0.5%]) in higher-income counties; in the lowest-income counties, the annual percentage change was 1.6% per year (95% CI = -0.7% to 4.0%). Counties with high smoking prevalence had marked increases in incidence compared with their counterparts (e.g., anal cancer among men increased 4.4% per year [95% CI = 2.7% at 6 .0%] for those living in counties with the highest smoking prevalence vs. 1.2% per year [95% CI = 0.7% to 1.7%] for those living in counties with the lowest smoking prevalence) . Improved, targeted prevention is needed to combat growing disparities. |
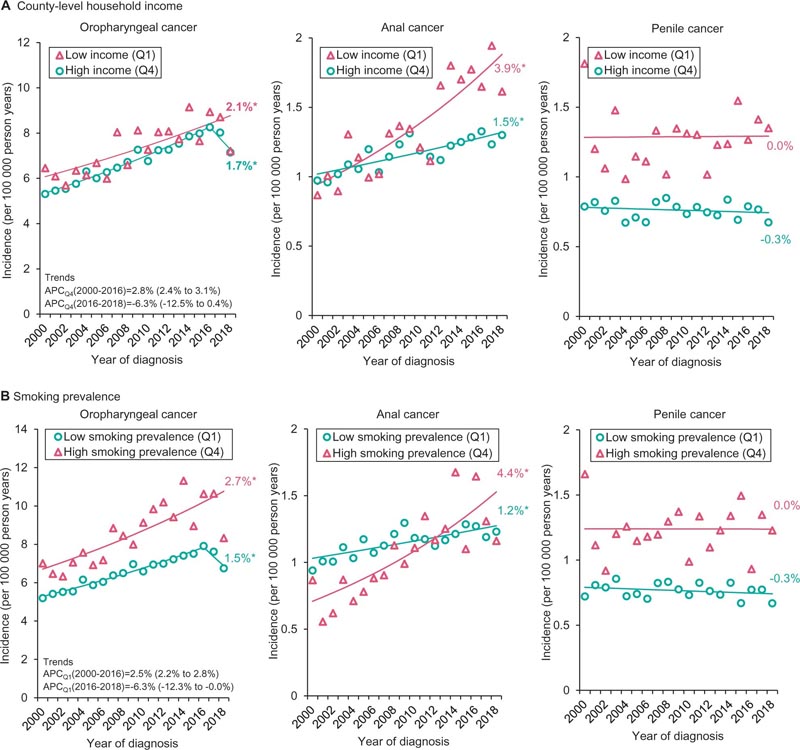
Incidence trends of human papillomavirus (HPV)-associated cancers by county-level household income and current smoking prevalence among men: Surveillance, Epidemiology, and End Results 21 (SEER-21; 2000-2018) . A) Trends in incidence rates (per 100,000 person-years) in HPV-associated cancers by highest and lowest income quartiles. B) Trends in incidence rates (per 100,000 person-years) in HPV-associated cancers by highest and lowest smoking prevalence quartiles. The values given along with the annual percentage changes (APC) in parentheses are the 95% confidence intervals. County-level income quartile values for men and women: Q1 = $9,330 to 29,640, Q4 = $39,410 to $82,930; county-level smoking prevalence for men: Q1 = 9.1% to 22.1%, Q4 = 29.3% to 44.7%; County-level smoking prevalence for women: Q1 = 2.9% to 18.3%, Q4 = 26.6% to 53.2%. *Statistically significant at P < 0.05 and all hypotheses were two-sided. A t test was used when there was no joining point and a z test when there were one or more joining points was used to determine the statistical significance of trends.
Discussion
Smoking has been identified as a risk factor for HPV-associated cancers. Although the exact mechanism of action remains unclear, smoking is thought to impair immune function, impeding the ability to clear HPV infection. Smoking can also inhibit apoptosis, promoting tumor growth.
Smoking and risky sexual behaviors are highly correlated with poverty.
Therefore, the marked increases in HPV-associated cancers in low-income counties could be attributed to a combined effect of smoking and increased HPV exposure.
The recent stabilization of cervical cancer incidence in high-income counties and reversal of the decline in incidence in low-income counties is concerning and needs further investigation. These trends are consistent with the stabilization of cervical cancer incidence observed nationally over a similar duration schedule in a recent study that used data from all US states and another study that documented the increase in incidence of cervical cancer in Puerto Rico.
The marked increases in the incidence of anal, oropharyngeal, and vulvar cancer combined with the high absolute incidence in low-income counties and those with a high prevalence of smoking are concerning. Currently, there are no evidence-based screening recommendations for these cancers; Therefore, its prevention is based solely on primary prophylaxis through vaccination against HPV.
While HPV vaccination coverage remains higher for adolescents below the poverty level, coverage in rural counties that generally have lower median household incomes is 15 percentage points lower than their counterparts. Without improvement in HPV vaccination coverage in low-income counties, these growing disparities are likely to worsen in future years.
The strength of our study is the use of high-quality data on county-level cancer incidence and income and smoking prevalence. The limitation of our study is that county-level data do not capture within-county variation in income and smoking prevalence and that individual-level inferences cannot be drawn from our analysis.
Additionally, to ensure data integrity, SEER allows a 22-month lag; however, reporting of cases diagnosed in an outpatient setting may be delayed. As a result, trends in more recent years may mistakenly appear to have declined.
In conclusion , the decline in cervical cancer incidence has begun to reverse, and marked increases in anal, oropharyngeal, and vulvar cancer incidence have occurred in disadvantaged counties. Targeted public health interventions are urgently needed to reduce growing disparities.
Comments
The incidence of cancers associated with the human papillomavirus (HPV) is beginning to rise, with larger increases seen in lower-income counties and counties with a high prevalence of smoking, according to research published in the issue April JNCI Cancer Spectrum.
Yueh-Yun Lin, of the UTHealth School of Public Health in Houston, and colleagues used the Surveillance, Epidemiology, and End Results 21 database to identify HPV-associated cancer between 2000 and 2018. Trends in incidence were calculated based on county-level income and smoking prevalence.
The researchers found that in lower-income counties, the incidence of anal and vulvar cancer among women and the incidence of anal cancer among men increased markedly, while in higher-income counties, the increases were slower ( e.g., for vulvar cancer, incidence increased 1.9 and 0.8 percent in the lowest and highest income counties, respectively).
Cervical cancer incidence has stabilized in higher-income counties in recent years (0.0 percent per year) and increased 1.6 percent per year in lower-income counties.
Notable increases in incidence were seen in counties with a high smoking prevalence compared to their counterparts (e.g., anal cancer increased by 4.4 vs. 1.2 percent per year among men living in counties with the highest versus lowest smoking prevalence).
"The decline in cervical cancer incidence has begun to reverse, and marked increases in anal, oropharyngeal, and vulvar cancer incidence occurred in disadvantaged counties," the authors write. "Specific public health interventions are urgently needed to reduce growing disparities."
















