Results
Our study included 1,635 records from 159 hospitals in 57 countries, collected between November 1, 2018 and January 31, 2020. 328 (20%) records were from countries in the very high HDI level, 539 (33%) of countries in the high HDI level, 614 (38%) of countries in the medium HDI level and 154 (9%) of countries in the low HDI level.
The median age was 35 years (IQR 24-51), with the oldest patients in the very high HDI level (median 54 years, IQR 34-69) and the youngest in the low HDI level ( median 28 years, IQR 20-38).
The most common procedures were elevation of a depressed skull fracture at the low HDI level (69 [45%]), evacuation of a supratentorial extradural hematoma at the mid HDI level (189 [31%]), and high HDI level (173 [32%]). %]), and the evacuation of a supratentorial acute subdural hematoma at the very high HDI level (155 [47%]).
The median time from injury to surgery was 13 h (IQR 6-32). Overall mortality was 18% (299 of 1635). After adjustment for casemix, the odds of mortality were higher at the medium HDI level (odds ratio [OR] 2.84, 95% CI 1.55–5.2) and the high HDI level (2.26 , 1.23– 4·15), but not the low level of the HDI (1·66, 0·61–4·46), in relation to the very high level of the HDI. There was significant variation between hospitals in mortality (median OR 2·04, 95% CI 1·17–2·49).
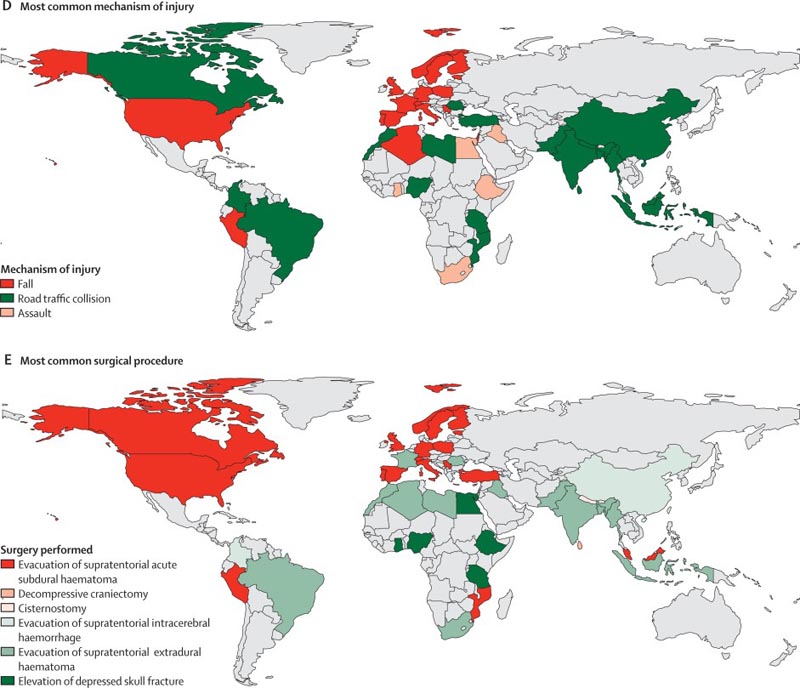
Cross-country variation in case mix by HDI category (A), age (B), admission GCS score (C), most common mechanism of injury (D), and most common surgical procedure (E) . Only countries with five or more patient registries are shown here (except panel A, which includes all countries contributing to the study). HDI=human development index. GCS=Glasgow Coma Scale.
Interpretation
Patients who received emergency neurosurgery for TBI differed considerably in their admission and management characteristics across developmental settings. The level of human development was associated with mortality.
Substantial opportunities were identified to improve care globally, including reducing delays in surgery. Between-hospital variation in mortality suggests that changes at the institutional level could influence the outcome and comparative effectiveness research could identify best practices.
Added value of the study
For the first time, the Global Neurotrauma Outcomes Study has captured the landscape of emergency neurosurgery for TBI worldwide.
There were significant differences in TBI case mix, management, and outcomes at all levels of human development. Patients at the low human development index (HDI) level were often young (median age 28 years) and had a mild traumatic brain injury with a depressed skull fracture due to an assault; at the medium HDI (median age 32 years) and high HDI (median age 35 years) levels, patients were also young but more often had a moderate or severe TBI with an extradural hematoma due to a traffic collision; and at the very high HDI level, patients were older (median age 54 years) and more frequently had moderate or severe TBI associated with acute subdural hematoma after a fall.
Quality of care was generally less favorable in lower human development settings, including temporal delays in surgery and lack of access to postoperative intracranial pressure monitoring and intensive care.
After adjustment for Casemix, level of human development was associated with mortality. The least favorable outcomes were seen at the mid-HDI level, which was likely because centers in these countries were dealing with a high volume of severely injured patients without access to the resources needed to care for them.
In particular, a relatively favorable outcome was observed at the low HDI level, which we postulated was due to a lower incidence of high-energy brain injuries in the general population and a higher proportion of severely injured patients who died before hospital. After adjustment for case mix and level of human development, there was still significant variation between hospitals in the outcome.
Implications of all available evidence The Global Neurotrauma Outcomes Study has identified significant heterogeneity in the epidemiology of emergency neurosurgery for TBI in developmental settings that has several implications.
|
Comments
Cambridge neurosurgery experts have led the largest-ever study examining the surgical management of traumatic brain injuries, highlighting regional inequalities in both the root causes and treatment of such injuries.
Largest study ever conducted on traumatic brain injuries highlights global inequality in causes and treatment
The NIHR-funded Global Neurotrauma Outcomes Study is published in The Lancet Neurology and provides data to aid decision-making and improve outcomes for patients with traumatic brain injury worldwide.
The document focuses on the types of cases, the way they are managed and mortality rates, and was compiled using data submitted by 159 hospitals in 57 countries to a central database, which the researchers then analyzed. The researchers stratified countries into four levels (very high, high, medium, low) based on their Human Development Index (HDI), which takes into account factors such as life expectancy, education and income.
The prospective study determined that patients in the low HDI level were often young and tended to suffer skull fractures due to assault, but were classified as having "mild" traumatic brain injury (TBI).
At the medium and high HDI levels, the patients were also young, but most had a moderate to severe traumatic brain injury caused by a traffic accident and an extradural hematoma, a hemorrhage on the outside of the dura mater, the membrane that covers the brain.
At the very high level, patients tended to be older and had moderate or severe traumatic brain injury associated with a fall and an acute subdural hematoma, a hemorrhage on the inner surface of the dura mater.
Overall, quality of care was less favorable in lower HDI settings, including delays in surgery and lack of postoperative monitoring and intensive care equipment.
The very high HDI level had the highest proportion of operations in which the most senior surgeon present in the operating room was a fully qualified neurosurgeon, while the medium HDI level had the lowest proportion. The study also found significant variations between hospitals in patient outcomes.
Angelos Kolias, consultant neurosurgeon at Cambridge University Hospitals NHS Foundation Trust (CUH) and associate director of the NIHR Global Neurotrauma Research Group, said: “The results show that overall mortality is low, reflecting the life-saving nature of surgery for traumatic brain injuries. Many of these patients would have died without an operation. However, we must also address deficits in pre-hospital management and long-term rehabilitation.”
David Clark, a neurosurgeon in training and researcher at the University of Cambridge, said: "A particularly important finding is that the outcome is more influenced by hospital characteristics than by country of origin, raising the possibility that changing systems and care processes at individual hospitals might be able to improve mortality. The document sows the seeds for discussion and change."
The research was funded by the NIHR using support from the UK government to support global health research.
Alexis Joannides, consultant neurosurgeon at CUH and informatics lead for the NIHR Global Neurotrauma Research Group, added: “The contribution of a number of clinicians and researchers from various hospitals around the world has been made possible by the infrastructure and collaborations supported by the NIHR.
“The database and data management process used in the study have now laid the foundation for a global traumatic brain injury registry that we have established to support continued quality improvement and research in the field of brain injury.” traumatic.”
Peter Hutchinson, professor of neurosurgery at the University of Cambridge and director of the NIHR Global Neurotrauma Research Group, said: "This is the world’s largest study looking at the surgical management of head injuries and will be of practical value to clinicians. and others with the purpose of planning strategies for the future.
“The collaboration between a large number of hospitals and countries, together with the support of the World Federation of Neurosurgical Societies and continental neurosurgical societies, has been phenomenal.”
Reference : Clark, D et al. Casemix, management, and mortality of patients receiving emergency neurosurgery for traumatic brain injury in the Global Neurotrauma Outcomes Study: a prospective observational cohort study. The Lancet Neurology; March 17, 2022; DOI: 10.1016/S1474-4422(22)00037-0
















