Key points How does comorbidity between mental disorders and general medical conditions affect life expectancy? Findings In this cohort study of 5,946,800 individuals, those with a mental disorder and general medical comorbidity had a higher risk of dying and a shorter life expectancy compared to the general population, patients with a mental disorder only, and those with conditions general medical only. . Meaning To reduce premature mortality in people with mental disorders, we must actively prevent and treat comorbid general medical conditions. Importance Premature mortality has been observed among people with mental disorders. Comorbid general medical conditions contribute substantially to this reduction in life expectancy. |
On average, people with mental disorders die earlier than those without them. Our recent study covering the Danish population showed that women and men with a mental disorder die 7 and 10 years earlier, respectively, than the general population of the same age and sex. Using state-of-the-art methods, we examine the contribution of different causes of death to the overall reduction in life expectancy in people with different mental disorders (e.g., mood disorders, schizophrenia, etc.).
For example, men diagnosed with substance use disorders have an average life expectancy that is 14.8 years shorter than the general population. While 5.4 years of this reduction is explained by suicides and unintentional injuries, the remainder (9.4 years) is due to general medical conditions (GMCs), such as diabetes or cardiovascular or respiratory diseases.
Other studies focusing on specific mental disorders have also reported that mortality rates from several general medical problems (GMCs) are higher among people with mental disorders, although they did not report absolute measures such as life expectancy.
The fact that a large portion of the mortality gap in people with mental disorders is related to GMCs is not unexpected, given that people with mental disorders are at higher risk of developing comorbid conditions. A recent study reported that people with mental disorders develop GMC earlier than those without mental disorders and were more likely to die younger than those without a mental or physical disorder.
While it is generally accepted that mental disorder-GMC comorbidity is a key factor underlying premature mortality, there are important gaps in the empirical evidence base. Previous studies have not comprehensively considered a wide range of mental disorder-GMC pairs, making it difficult to establish pairwise comparisons, or have not provided sex-specific estimates.
Additionally, research has focused on mortality rates (MRR) or other relative measures, but in recent years, health metrics to assess premature mortality have developed greatly. Using both types of measures provides a more complete picture of the mortality associated with these disorders and their comorbidity.
Aim
Provide an analysis of mortality associated with comorbidity among a wide range of mental disorders and general medical conditions.
Design, environment and participants
Population-based cohort study of 5,946,800 people born in Denmark between 1900 and 2015 and residing in the country at the start of follow-up (January 1, 2000 or their date of birth, whichever occurred later).
Exhibitions
Danish health registries were used to identify people with mental disorders and general medical conditions.
Main results and measures
Considering pairs of mental disorders and general medical conditions, we calculated mortality rate ratios (MRR) and differences in life expectancy (i.e., years of life lost) to assess the association of mortality with both disorders of interest compared with the mental disorder of interest, the general medical condition of interest, and no disorder of interest.
Results
The study population was composed of 2,961,397 men and 2,985,403 women, with a median age (IQR) of 32.0 years (7.3-52.9) at the beginning of follow-up and 48.9 years (42. 5-68.8) at the end.
Based on all pairs of comorbid mental disorders and general medical conditions, the mean MRR compared to people without these conditions was 5.90 (median, 4.94; IQR, 3.80-7.30), and the mean reduction in life expectancy compared to the general population was 11.35 years (median, 11.08; range, 5.27-23.53; IQR, 8.22-13.72).
The association with comorbidity of general medical status in people with mental disorders varied by general medical status; For example, the addition of a neurological condition for each of the mental disorders was associated with a mean MRR of 1.22, while for cancer, the mean MRR for all mental disorders was 4.07.
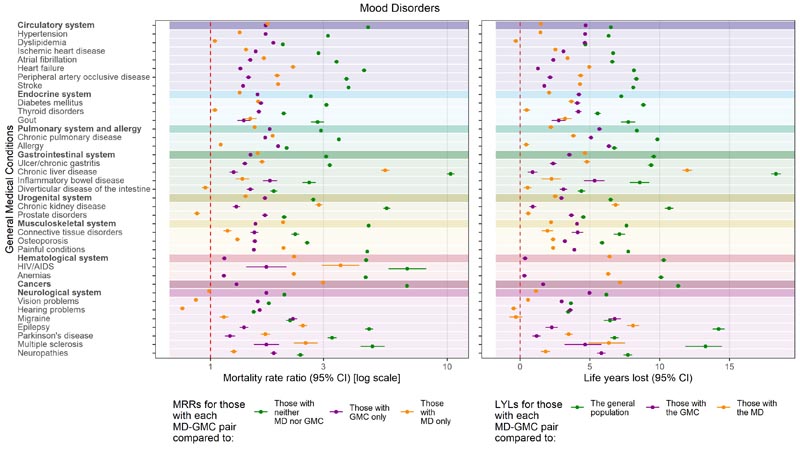
Using both mortality rate (MRR) and years of life lost (LYL), we observed shorter life expectancies for people with comorbid mental disorder and general medical condition.
The MRR and LYL for mood disorders are shown below:
Conclusions and relevance
In this study, shorter life expectancy was associated with comorbid mental disorders and general medical conditions compared to the total population and also to patients who had only mental disorders or only general medical conditions. Prevention and early detection of comorbidities could reduce premature mortality in patients with mental disorders.
Discussion
This population-based study provides detailed estimates of mortality associated with GMC-mental disorder comorbidity. We believe these estimates provide the most detailed assessments of the association with comorbid GMC among people with mental disorders.
We want to highlight 3 key findings:
First, MRRs were elevated for all disorder pairs compared to people without any disorder; the mean mortality rate for those who had both disorders in the mental disorder-GMC pair of interest compared with people who had neither disorder was almost 6 times higher. Compared to people who only had the mental disorder of interest or only the GMC of interest, it was more than twice as high. Therefore, regardless of the type of mental disorder or GMC, comorbidity between mental disorders and GMCs is widely associated with substantially higher MRR.
Second, some disorders affect mortality rates more than others. Considering the association with the addition of a GMC (compared to just the mental disorder of interest), the highest mean MRRs were observed for the addition of cancer (4.07) and hematologic GMCs (2.67). This is consistent with the overall lethality of these disorders; however, regardless of the type of GMC, MRRs were increased. Considering the association with the addition of a mental disorder (compared to just the GMC of interest), the highest mean MRRs were observed for the addition of eating disorders (3.23) and substance use disorders (3.23). 05). It should be noted that for some combinations of specific mental disorders and GMC (e.g., various mental disorders and dyslipidemia, allergy, migraine, vision problems, and hearing problems), mortality was lower among those with GMC and mental disorder, compared to people who only had the mental disorder. While this finding may be due to chance for some pairs, there may be GMC-specific reasons for these observations.
Third, life expectancy was 11.5 years shorter in people with comorbid mental disorders and GMC compared to life expectancy in the general population. The contribution of different GMCs to premature mortality in people with MD varied, but for some pairs it was substantial; The reduction in life expectancy ranged from 1.5 months (organic disorders and neurological GMC) to 16 years (behavioral disorders and cancer). Similarly, the addition of a mental disorder in people with GMC ranged from 2.5 months (intellectual disorders and hematological GMC) to 12 years (intellectual disorders and neurological GMC).
The association between mental disorders and premature mortality is well established. Previous articles recognize that although some premature mortality in people with serious mental disorders could be attributed to external causes (e.g., suicide, accidents), a substantial proportion of premature mortality was attributable to GMC comorbidity, particularly diseases heart disease, diabetes, cancer and chronic obstructive pulmonary disease. A study of veterans with type 2 diabetes found that the risk of death increased with increasing GMC comorbidity, regardless of the number of psychiatric conditions.
Our article highlights that among people with a mental disorder, the addition of a GMC was generally associated with increased premature mortality ; however, the addition of mental disorders in those with GMC also reduces life expectancy. Although the MRR and LYL analyzes effectively consider the same associations, that is, the association with the addition of a GMC, a mental disorder, or both, the magnitude of the results for the 3 comparisons does not always follow the same pattern. It should be remembered that the MRR and LYL use different comparison groups.
Our study uses the Danish national registries, which provide a large sample size. These data limit recall and self-report bias. Because data were available on the entire population and Danish citizens have free and equal access to healthcare, selection bias is minimized.
Final message Using anonymized data from 5.9 million people living in Denmark, we investigated how comorbidity between mental disorders and general medical conditions affects life expectancy. We found that people with comorbid mental disorders and general medical conditions have a higher risk of dying and a shorter life expectancy compared to: To the population in general. b) Only those with mental disorders. c) Those with general medical conditions only. Our findings highlight that people with GMC-mental disorder comorbidity have a higher risk of dying; Their life expectancy is shorter than that of the entire population and that of people with mental disorders or GMC only. Physical-mental multimorbidity is increasing and represents a challenge to healthcare systems worldwide; It is associated with high utilization of health services, costs and social inequality. Logically, it follows that early identification and good management of mental disorders, as well as prevention of GMC comorbidity, could help reduce part of the risk of premature mortality in people with mental disorders. Prevention and early detection of comorbidity could help reduce the association with mortality, and several studies have shown a reduction in mortality with good management of mental disorders. However, reviews of interventions to address GMCs and risk behaviors have concluded that health outcomes improve if interventions can target risk factors such as depression in people with comorbidity. Although some well-designed interventions appear to be effective in reducing risk factors in people with severe mental disorders, the evidence was low for most interventions. We hope that these estimates provide a basis for future research aimed at improving life expectancy among people with comorbidity. They highlight the need to optimize GMC screening among people with mental disorders so that comorbidity can be prevented or identified early and managed well. |
















