Highlights
|
Introduction
The incidence of myocardial infarction has decreased in several populations since the middle of the last century, due to a reduction in traditional risk factors for atherosclerotic cardiovascular disease and the establishment of new effective treatments for primary and secondary prevention in randomized trials. However, historically, women and the elderly were underrepresented in cardiovascular prevention research and have differential risk factors for atherosclerotic cardiovascular disease compared with men and younger people.
The most recent studies on the incidence of myocardial infarction were followed until the mid-2010s, or reported age- and sex-standardized incidences, and thus do not show age- and sex-specific developments in the incidence of myocardial infarction. .
Therefore, it is unclear whether the declining incidence of myocardial infarction from the 1950s to the mid-2010s has continued into the current decade and whether it applies specifically to women and the elderly. To address this knowledge gap, we conducted a national, registry-based study of age- and sex-specific trends in the incidence of first myocardial infarction in Denmark from 2005 to mid-2021.
Background and objectives
Few studies have determined whether the declining incidence of myocardial infarction continues in the current decade and how it is affected by age and sex. Our objective was to determine age- and sex-specific changes in the incidence of myocardial infarction in Denmark from 2005 to 2021.
Methods
First admissions for myocardial infarction in adults aged ≥18 years were identified through Danish national registries.
Incidence rates per 100,000 people with 95% confidence intervals (CI) were calculated by calendar year, sex, and age groups (≤49, 50–69, 70–84, ≥85 years).
We also present incidence rate ratios (IRRs) with 95% CIs for 2019–2021 compared to 2005–2007.
Results
From January 1, 2005 to August 4, 2021, there were 116,481 incident acute myocardial infarctions in approximately 4.5 million Danes aged ≥18 years.
The overall incidence rate of myocardial infarction per 100,000 people decreased in both sexes from 2005 to 2021 (women: 143 to 80; men: 243 to 174) and in all age groups.
The steepest declines in incidence were observed for ages ≥85 years (men: 55%, IRR: 0.45 [0.41–0.49]; women: 58%, IRR: 0.42 [0.39– 0.45]) and 70–84 years (men: 46%, IRR: 0.54 [0.52–0.57]; women: 52%, IRR: 0.48 [0.46–0.51] ).
Rates also decreased significantly for ages 50 to 69 years (men: 19%, IRR: 0.81 [0.79–0.84]; women: 17%, IRR: 0.83 [0.78–0.84] .88]) and ≥49 years (men: 30%, IRR: 0.70 [0.64-0.76]; women: 37%, IRR: 0.63 [0.54-0.74]).
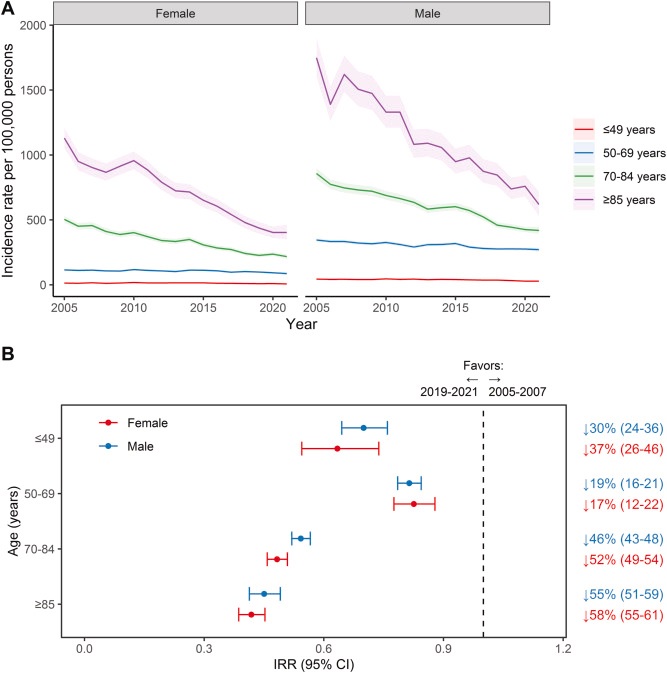
Figure 1 (A) Incidence rate of myocardial infarction per 100,000 people with 95% confidence intervals, 2005-2021. (B) Relative changes in the incidence of first myocardial infarction during the period 2019-2021 compared to the period 2005-2007 (reference), presented as incidence rate ratios and percentages with 95% confidence intervals. ↓ = decrease; CI = confidence intervals; IRR = incidence rate ratio.
Conclusions
Declines in the incidence of myocardial infarction continued in the current decade in all age and sex groups. However, significantly steeper absolute and relative declines were observed among older age groups (≥70 years).
Discussion
Our study provides a contemporary estimate of the age- and sex-specific incidence of first myocardial infarction in a national setting. Using Danish registries with national coverage, we identified gaps in the rate of decline in the incidence of myocardial infarction between age groups.
We observed a steeper decline among older age groups (≥70 years) compared to the young and middle-aged.
Although the incidence rate remained higher among men and the median age of onset remained higher among women, both sexes experienced similar decreases in the incidence of myocardial infarction.
Our findings highlight the need to intensify the focus on cardiovascular prevention in the young and middle-aged population. Furthermore, contemporaneous age- and sex-specific rates are useful for updating background information in clinical trials, as well as for updating and calibrating risk prediction models.
Declines in the incidence of myocardial infarction over the previous century were primarily among younger people, leading to a shift in the burden of coronary heart disease toward older age groups.
In contrast to this phenomenon, our findings suggest that between 2005 and 2021, the median age at first myocardial infarction has remained relatively stable, and that middle to older age groups, rather than the elderly, need a focus additional preventative in the future. This is underlined by the divergent development in the use of statins before myocardial infarction. To our knowledge, the present study is the only one that reports such a contrast in the relative decrease in the incidence of myocardial infarction in the elderly. Therefore, our findings require corroboration in other populations and data sources.
Our findings build on previous studies, which showed decreases in the incidence of myocardial infarction in several populations and several decades. These improvements are likely related to better control of risk factors and greater acceptance of preventive treatment based on evidence.
We find that these developments extend into the current decade. However, we observed stable rates of myocardial infarction incidence among the youngest (≤69 years) until around 2014, while the incidence steadily decreased among the oldest (≥70 years) from 2005 to 2021. Where the oldest iterations While international prevention guidelines focused primarily on the middle-aged population, more attention has been paid to cardiovascular prevention throughout life.
This was reflected in the proportion of statin use before myocardial infarction in our study population, which remained stable for the younger groups and increased steeply for the older groups. As such, our findings may represent a lag in prevention among the elderly during the 1990s and 2000s, that is, the greater relative and total decline observed among the elderly during the study period may represent a catch-up effect.
However, this only suggests a partial and speculative explanation of our findings, while temporal developments in the distribution of myocardial infarction risk factors, such as smoking, blood pressure, and physical activity, may also have played a role. important role, but unfortunately those data were not available in our study.
Another explanation for our findings could be, as mentioned, that diagnostic sensitivity had improved. If this improvement had differential effects between age groups, that is, greater diagnostic sensitivity led to more myocardial infarctions detected in the younger, but not in the older, this may explain part of the observed discrepancy. However, as mentioned, we would expect the opposite to happen, that is, more heart attacks would be detected among the elderly. Unfortunately, data on diagnostic findings such as troponin were not available . In any case, notably, after 2014, incidence continued to decline for younger people as of this writing.
Furthermore, the observed steeper relative decline in the incident rate of myocardial infarction among the elderly may have been affected by concomitant increasing long-term survival. Therefore, secondary prevention in the elderly still requires significant attention, despite the large improvements in the incidence of first-time myocardial infarction described in our study.
Final message The incidence of myocardial infarction decreased from 2005 to 2021 by age and sex, but was marked by a steeper decline among those over 70 years of age. Continued focus on risk factor modification and preventive intervention could further reduce the incidence of myocardial infarction in the future. |
















