Highlights
|
Introduction
Type 2 myocardial infarction (MI) results from an imbalance in myocardial oxygen supply/demand.
For example, patients with hypotension secondary to gastrointestinal bleeding may develop myocardial ischemia sufficient to produce myocardial necrosis. Such patients may or may not have clinically relevant atherosclerotic coronary artery obstruction.
It stands to reason that a patient with clinically significant coronary artery stenosis would be at increased risk of developing type 2 myocardial infarction under appropriate conditions, such as hypotension, bradycardia, or tachycardia .
In this study, the authors evaluated 100 patients with type 2 myocardial infarction. Two-thirds of these individuals had coronary artery disease (CAD) and one-third had left ventricular dysfunction (LVD). The presence of clinically significant CAD or LVD had not been observed or treated before the onset of type 2 MI.
The study suggests that patients with type 2 myocardial infarction should, at some point, undergo invasive or noninvasive evaluation for CAD and/or LVD, and if discovered, appropriate evidence-based therapy should be initiated.
Background
Type 2 myocardial infarction is caused by an imbalance between myocardial oxygen supply and demand, and its diagnosis is becoming more common with the advent of highly sensitive cardiac troponin assays.
Although this diagnosis is associated with poor outcomes, widespread uncertainty and confusion remains among clinicians about how to investigate and manage this heterogeneous group of patients with type 2 myocardial infarction.
Methods
In a prospective cohort study, 8064 consecutive patients with elevated cardiac troponin concentrations were examined to identify patients with type 2 myocardial infarction.
Patients with frailty or renal or hepatic insufficiency were excluded . All study participants underwent coronary (CT or invasive angiography) and cardiac (MRI or echocardiography) imaging, and the underlying causes of the infarction were independently adjudicated. The primary outcome was the prevalence of coronary artery disease.
Results
In 100 patients with a provisional diagnosis of type 2 myocardial infarction (median age, 65 years [interquartile range, 55-74 years]; 57% women), coronary and cardiac imaging reclassified the diagnosis in 7 patients: type 2 myocardial infarction 1 or 4b in 5 and acute myocardial injury in 2 patients.
In those with type 2 myocardial infarction, median cardiac troponin I concentrations were 195 ng/L (interquartile range, 62–760 ng/L) at presentation and 1165 ng/L (interquartile range, 277–3782 ng /L) in repeated tests.
The prevalence of coronary artery disease was 68% (63 of 93), being obstructive in 30% (28 of 93). Late gadolinium enhancement with infarct pattern or regional wall motion abnormalities were seen in 42% (39 of 93), and left ventricular systolic dysfunction was seen in 34% (32 of 93).
Only 10 patients had normal coronary and cardiac images. Coronary artery disease and left ventricular systolic dysfunction were previously unrecognized in 60% (38 of 63) and 84% (27 of 32), respectively, with only 33% (21 of 63) and 19 % (6 of 32) with evidence-based treatments.
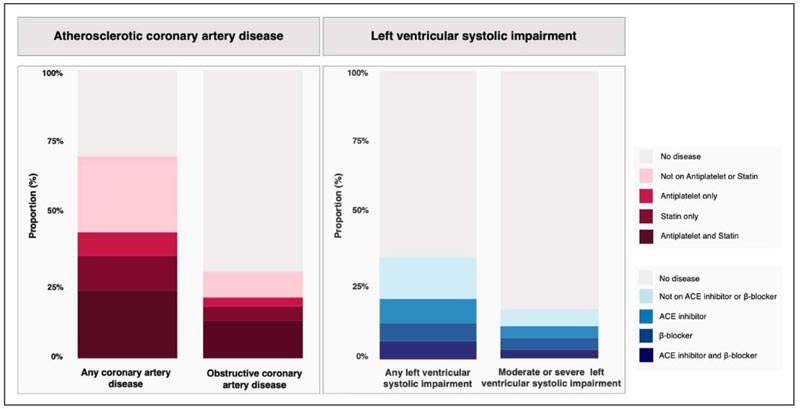
Previous treatment in patients with coronary artery disease and left ventricular systolic impairment identified on coronary and cardiac imaging. Proportion of patients with coronary artery disease or left ventricular failure identified on coronary and cardiac imaging, respectively, stratified by prior treatment with evidence-based medical therapy. ACE indicates angiotensin-converting enzyme.
Conclusions
|
What’s new?
DEMAND-MI (Determining the Mechanism of Myo-cardial Injury and Role of Coronary Disease in Type 2 Myocardial Infarction ) is the first prospective study to perform systematic cardiac imaging in 100 patients with type 2 myocardial infarction.
• Cardiac imaging led to diagnostic reclassification in 7 of 100 patients.
• In those with confirmed type 2 myocardial infarction, two-thirds had coronary artery disease and one-third had left ventricular failure, which were previously unrecognized and untreated in the majority.
•Less than half of all patients with an adjudicated diagnosis of type 2 myocardial infarction had a myocardial scar or regional wall motion abnormalities on imaging, usually associated with myocardial infarction.
What are the clinical implications?
• In patients with type 2 myocardial infarction, investigation with invasive or noninvasive coronary and cardiac imaging should be considered because identification of unrecognized coronary artery disease and left ventricular impairment will have immediate and long-term implications for treatment.
• In those patients without imaging evidence of myocardial infarction or coronary artery disease, the patient is unlikely to benefit from therapies directed at coronary atherosclerosis; In this context, the value of a diagnosis of type 2 myocardial infarction is questionable.
















