Effect of bariatric surgery on the risk of complications after total knee arthroplasty. A randomized clinical trial
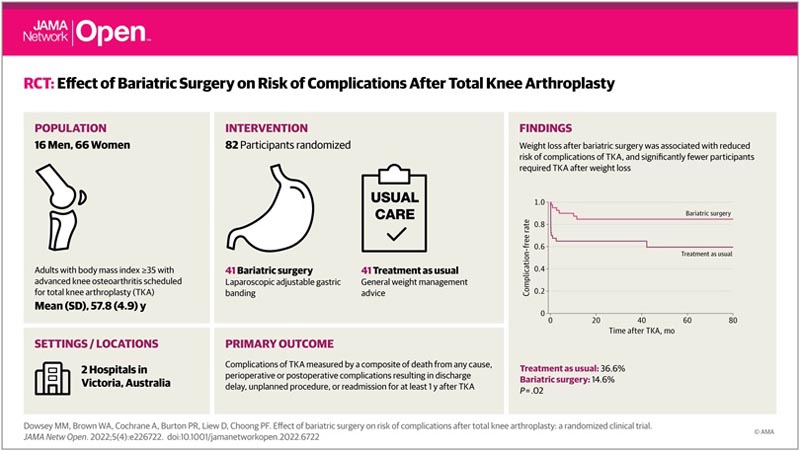
Key points Does bariatric surgery reduce the risk of complications after total knee arthroplasty (TKA) in patients with severe obesity? Findings In this randomized clinical trial of 82 adults aged 65 years or younger with class II obesity, those who were scheduled to undergo total knee arthroplasty experienced fewer joint surgery complications after undergoing a bariatric procedure, compared to those who underwent total knee arthroplasty without weight loss intervention. Meaning The findings suggest that people with severe obesity and knee osteoarthritis should seek to lose weight before considering TKA, and weight loss appears to reduce complications from joint surgery. |
Importance
People with severe obesity who undergo total knee arthroplasty (TKA) for osteoarthritis (OA) are at increased risk of short- and long-term complications compared to people with a baseline body mass index (BMI) ( <30); weight in kilograms divided by height in meters squared). It is not known whether weight loss before TKA modifies this risk.
Aim
To determine whether outcomes are improved by undergoing bariatric surgery before TKA in people with a BMI greater than or equal to 35 and end-stage OA.
Design, scope and participants
This randomized, evaluator-blind, parallel-group clinical trial was conducted between May 2012 and June 2020 with a minimum follow-up of 12 months after total knee arthroplasty.
TKA was performed at a public hospital affiliated with a tertiary referral university, and bariatric surgery was performed at a private hospital center and a private practice affiliated with the university. Data analysis was carried out from February to July 2021.
Interventions
Bariatric surgery compared with usual weight management counseling (treatment as usual [TAU]) in patients scheduled for TKA.
Main results and measures
The primary outcome was TKA complications measured by a composite of death from any cause, perioperative or postoperative complications resulting in a delay in discharge, an unplanned procedure, or readmission for at least 12 months after TKA.
Secondary outcomes included hospital bed day utilization, anthropomorphic measures, and patient-reported outcomes.
Results
Eighty-two patients awaiting TKA were randomized to undergo bariatric surgery (41 patients) or TAU (41 patients). Of the 82 participants, 66 (80.5%) were women, the mean (SD) age was 57.8 (4.9) years, and the mean (SD) BMI was 43.8 (5.5).
Thirty-nine participants (95.1%) in the intervention group underwent laparoscopic adjustable gastric banding and 29 (70.7%) subsequently underwent TKA.
Thirty-nine patients (95.1%) in the TAU group underwent TKA.
Six patients (14.6%) in the intervention group incurred the primary outcome (median follow-up, 24 months), compared with 15 (36.6%) in the TAU group (median follow-up, 27 months) ( difference, 22.0%; 95% CI, 3.7% to 40.3%, P = 0.02).
The between-group difference in BMI at 12 months was −6.32 (95% CI, −7.90 to −4.50; P < .001) in favor of the intervention group 12 participants (29.3% ) in the intervention group refused TKA due to symptom improvement, while 2 participants (4.9%) in the TAU group refused TKA (difference, 24.4%; 95% CI, 9. 0% to 39.8%; P = .003).
Discussion
In this evaluator-blind RCT, among patients with severe obesity and knee OA who underwent TKA, significantly fewer patients who underwent bariatric surgery experienced a post-TKA complication compared with those who underwent ATR alone.
The main factor associated with this difference was the group of participants (30.8%) who declined to undergo total knee arthroplasty due to symptom improvement with weight loss after the bariatric procedure. This was despite participants meeting clinical and radiographic criteria for TKA at initial clinical evaluation.
To our knowledge, this is the first RCT evaluating the effectiveness of substantial weight loss induced by bariatric surgery in reducing the risk of complications after TKA in patients with severe obesity and knee OA.
In previous uncontrolled studies of bariatric surgery before TKA, findings have been equivocal. A lower risk of complications and death has been recorded in patients undergoing bariatric surgery before TKA, and yet the opposite has also been described. Possible explanations for the inconsistent findings include inaccuracies with retrospective review of medical records and incomplete capture of data arising from short-term follow-up.
A surprising finding of our study was that almost one-third of patients had not proceeded with planned TKA until 5 years after bariatric surgery.
Although not the primary intent of our study, these results indicate that for a substantial portion of patients with severe obesity and knee osteoarthritis, symptoms can be effectively controlled with weight loss strategies alone. This is supported by a previous smaller study 5 that demonstrated a positive association between BMI change and pain and functional improvement 6 months after bariatric surgery in patients with severe obesity and knee OA, with patients inclined to defer surgery. ATR.
Conclusions and relevance
|
















