Key points Is traumatic brain injury associated with long-term risk of cardiometabolic, neurological, or psychiatric comorbidities? Findings In this cohort study including 4351 patients each with mild or moderate to severe TBI and 4351 frequency-matched unexposed patients without TBI, the rates of cardiovascular and endocrine comorbidities after TBI were significantly higher in patients with mild or moderate to severe TBI. moderate to severe compared to patients without TBI. The risk of post-TBI comorbidities was higher in all age groups compared with age-matched unexposed patients, particularly in patients younger than 40 years, and post-TBI comorbidities were associated with increased mortality during a follow-up period of 10 years. Meaning These findings suggest that TBI patients in all age groups may benefit from a proactive targeted screening program for chronic multisystem diseases, particularly cardiometabolic diseases, after injury. |
Introduction
Traumatic brain injury (TBI) is a global health problem, with an estimated incidence of 64 to 74 million cases per year worldwide and is a leading cause of morbidity and mortality. Poor clinical outcomes may be due to direct sequelae of TBI, prior comorbidities, or a combination of these factors. Additionally, large-scale studies of American football players and military veterans have shown that prior traumatic brain injury is associated with chronic multisystem conditions , suggesting that recurrent severe head injuries may be associated with health and functional status. long-term.
The development of chronic medical comorbidities after TBI can complicate the course of recovery and increase healthcare costs and mortality. A number of registry-based studies have demonstrated an increased risk of cardiovascular and metabolic disorders as well as epilepsy, stroke, and depression in the chronic phase of TBI recovery.
However, most previous studies were based on self-report, focused on older age groups, or included patients with TBI and preexisting comorbidities, which prevented isolating the association of TBI severity with the subsequent development of comorbidities and mortality. particularly in individuals who were otherwise healthy at the time of injury.
In a 2021 study we found an increased risk of developing multisystem medical and behavioral comorbidities in previously healthy patients who suffered a concussion. Notably, the risk of post-concussive comorbidities was higher in patients younger than 40 years compared to age-matched unexposed patients.
However, it is unclear whether our findings apply to more severe subtypes of TBI and whether subsequent comorbidities are associated with mortality risk. A better understanding of the interaction between TBI and the development of medical and neurological comorbidities may have important implications for preventive care, prognosis, and screening in a high-risk population.
Here we present the results of a large observational study of age-, race-, and sex-matched cohorts over a 10-year period to evaluate the risk and timing of cardiovascular, endocrine, psychiatric, and neurological diagnoses in people with mild TBI (mLCT) and TBI. moderate to severe (mLCT) compared with individuals without traumatic brain injury, considered unexposed patients, and evaluate the association between post-TBI comorbidities and mortality after hospital discharge.
Importance
The increased risk of neurological and psychiatric conditions following traumatic brain injury (TBI) is well defined. However, the risk of cardiovascular and endocrine comorbidity after TBI in individuals without these comorbidities and associations with post-TBI mortality have received little attention.
Aim
To evaluate the incidence of cardiovascular, endocrine, neurological, and psychiatric comorbidities in patients with mild TBI (mTBI) or moderate to severe TBI (mTBI) and analyze the associations between post-TBI comorbidities and mortality.
Design, environment and participants
This prospective longitudinal cohort study used data from hospital patient records from a tertiary academic medical center to select patients without prior clinical comorbidities who suffered from LCI between 2000 and 2015.
Using the same data registry, individuals without head injuries, the unexposed group, and without target comorbidities were selected and matched by age, sex, and racial frequency to the TBI subgroups. Patients were followed for up to 10 years . The data was analyzed in 2021.
Exhibitions
Mild or moderate to severe head trauma.
Main results and measures
Cardiovascular, endocrine, neurological, and psychiatric conditions were defined based on the International Classification of Diseases, Ninth Revision (ICD-9) or the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). Associations between TBI and comorbidities, as well as associations between comorbidities and mortality, were analyzed.
Results
A total of 4351 mLCT patients (median [IQR] age, 45 [29-57] years), 4351 mLCT patients (median [IQR] age, 47 [30-58] years), and 4351 unexposed individuals (median [IQR] IQR] age, 46 [30-58] years) were included in the analyses.
In each group, 45% of the participants were women. mLCT and msLCT were significantly associated with increased risks of cardiovascular, endocrine, neurological, and psychiatric disorders compared to unexposed individuals.
Notably, the risk of hypertension was increased in the mLCT (HR, 2.5; 95% CI, 2.1-2.9) and msTBI (HR, 2.4; 95% CI, 2.0-2.9) groups. 2.9).
The risk of diabetes was increased in the mLCT (HR, 1.9; 95% CI, 1.4-2.7) and msLCT (HR, 1.9; 95% CI, 1.4-2.6) groups. ), and the risk of ischemic stroke or transient ischemic attack also increased in mLCT (HR, 2.2; 95% CI, 1.4-3.3) and msLCT (HR, 3.6; 95% CI) groups. %, 2.4-5.3).
All comorbidities in the TBI subgroups emerged within a median (IQR) of 3.49 (1.76-5.96) years after injury.
Risks for post-TBI comorbidities were also higher in patients aged 18 to 40 years compared with age-matched unexposed individuals: the risk of hypertension was increased in mTBI (HR, 5.9; 95% CI). 3.9-9.1) and mTBI (HR, 3.9). ; 95% CI, 2.5-6.1), while hyperlipidemia (HR, 2.3; 95% CI, 1.5-3.4) and diabetes (HR, 4.6; 95%, 2.1-9.9) increased in the TBI group.
People with msLCT, compared with unexposed patients, had an increased risk of mortality (432 deaths [9.9%] vs. 250 deaths [5.7%]; risk of hypertension was increased in the mLCT groups (HR , 5.9; 95% CI, 3.9-9.1) and msTBI (HR, 3.9; 95% CI, 2.5-6.1), while hyperlipidemia (HR, 2. 3; 95% CI, 1.5-3.4) and diabetes (HR, 4.6; 95% CI, 2.1-9.9) were increased in the mLCT group.
People with msLCT, compared with unexposed patients, had an increased risk of mortality (432 deaths [9.9%] vs. 250 deaths [5.7%]; risk of hypertension was increased in the mLCT groups (HR , 5.9; 95% CI, 3.9-9.1) and msLCT (HR, 3.9; 95% CI, 2.5-6.1), while hyperlipidemia (HR, 2. 3; 95% CI, 1.5-3.4) and diabetes (HR, 4.6; 95% CI, 2.1-9.9) were increased in the mLCT group.
Individuals with msTBI, compared with unexposed patients, had an increased risk of mortality (432 deaths [9.9%] vs. 250 deaths [5.7%]; p < 0.001); post-injury hypertension (HR, 1.3; 95% CI, 1.1-1.7), coronary artery disease (HR, 2.2; 95% CI, 1.6-3.0) and adrenal insufficiency (HR, 6.2; 95% CI, 2.8-13.0) were also associated with increased mortality.
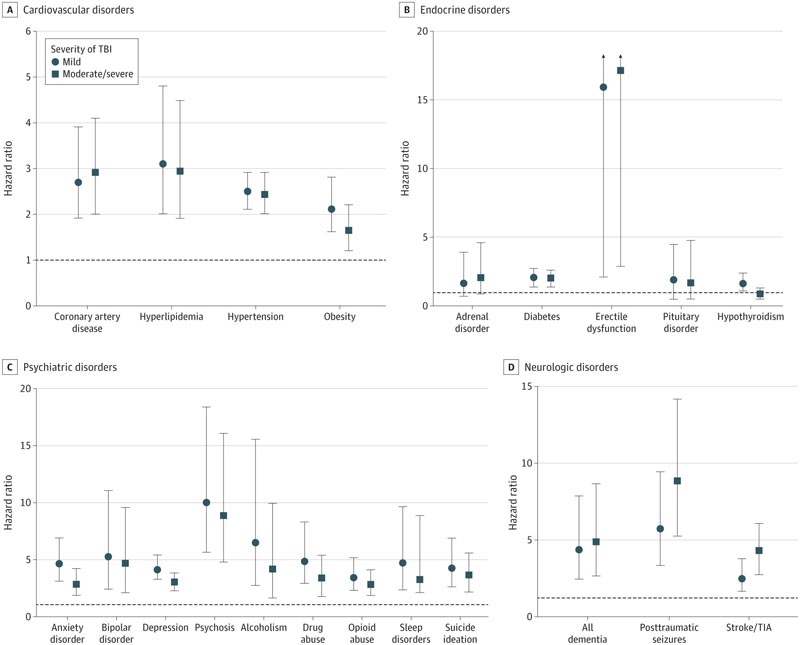
Risks of multisystem comorbidities after traumatic brain injury (TBI) stratified by severity
Conclusions and relevance
|
















