The Impact of Inflammation from the Initial Episode of COVID-19 Among Adults on Mortality within 12 Months of Hospital Discharge Background: Inflammation in the initial episode of COVID-19 may be associated with post-recovery mortality. The objective of this study was to determine the relationship between systemic inflammation in adults hospitalized with COVID-19 and mortality after recovery from COVID-19. Methods: An analysis of patient electronic health records (EHR) from January 1, 2020 to December 31, 2021 was performed for a cohort of hospitalized COVID-19-positive adult patients. 1207 patients were followed for 12 months after the COVID-19 episode in a health system. The 12-month mortality risk associated with inflammation, C-reactive protein (CRP), was assessed in Cox regressions adjusted for age, sex, race, and comorbidities. Analyzes assessed whether steroids prescribed at discharge were associated with subsequent mortality. Results: Elevated CRP was associated with other severity indicators of COVID-19 hospitalization, including supplemental oxygen and intravenous dexamethasone. Elevated CRP was associated with a higher risk of mortality after recovery from COVID-19. This effect was present for the unadjusted (HR = 1.60; 95% CI: 1.18, 2.17) and adjusted (HR = 1.61; 95% CI: 1.19, 2.20) analyzes ) when CRP was divided into high and low groups at the median. Oral steroid prescriptions at discharge were found to be associated with a lower risk of death after discharge (adjusted HR = 0.49, 95% CI: 0.33 to 0.74). Discussion: The hyperinflammation present with severe COVID-19 is associated with an increased risk of mortality after hospital discharge. Although suggestive, treatment with anti-inflammatory medications such as steroids at the time of hospital discharge is associated with a decreased risk of post-acute mortality from COVID-19. |
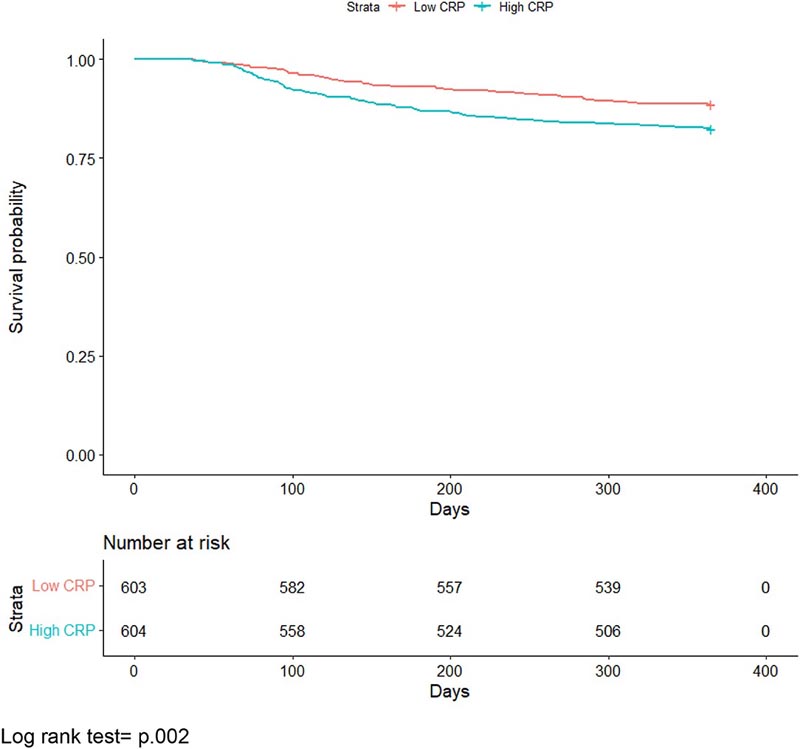
All-cause mortality Kaplan-Meier curve comparing individuals with average or higher C-reactive protein levels versus levels below the median. Log rank test = p.002.
Comments
Evidence continues to gather that ’Long Covid’ , that is, ongoing negative health impacts months after apparent recovery from severe Covid-19, is a significant risk for some patients. For example, researchers at the University of Florida in Gainesville showed last December that hospitalized patients who apparently recovered from severe Covid-19 are more than twice as likely to die in the next year, compared to people who only experienced mild or moderate symptoms and who had not been hospitalized, or who never contracted the disease.
Common steroids after ’long Covid recovery’ can reduce risk of death by up to 51%
Now, a team including some of the same authors shows, for the first time, that among patients hospitalized with Covid-19 who apparently recovered, severe systemic inflammation during their hospitalization is a risk factor for death within a year . This may seem paradoxical, since inflammation is a natural part of the body’s immune response, which has evolved to fight infections. But in some diseases, including Covid-19, this response can be exceeded and cause more damage.
“Covid-19 is known to create inflammation, particularly during the first acute episode. Our study is the first to examine the relationship between inflammation during Covid-19 hospitalization and mortality after the patient has "recovered," said first author Professor Arch G Mainous III, vice president of research at the Department. of Community Health and Family Medicine. at the University of Florida Gainesville.
"Here we show that the stronger the inflammation during initial hospitalization, the greater the likelihood that the patient will die within 12 months after apparently ’recovering’ from Covid-19."
Mainous and colleagues studied the anonymized electronic health records of 1,207 adults hospitalized in 2020 or 2021 after testing positive for Covid-19 within the University of Florida health system, and who had been followed for at least a year after the high. As an indicator of the severity of systemic inflammation during hospitalization, they used a common and validated measure, the blood concentration of the C-reactive protein (CRP) molecule, secreted by the liver in response to a signal from active immune cells.
Inflammation in many parts of the body.
As expected, the concentration of CRP in blood during hospitalization was strongly correlated with the severity of Covid-19: 59.4 mg/L for hospitalized patients 126.9 mg/L for those who required extra oxygen through ventilation non-invasive non-mechanical, and 201.2 mg/L for the most severe cases, which required ventilation through a ventilator or through extracorporeal membrane oxygenation.
Covid-19 patients with the highest CRP concentration measured during their hospital stay had a 61% higher risk, corrected for other risk factors, of dying from any cause within a year of hospital discharge than patients with the lowest concentration of CRP. These results are published in Frontiers in Medicine.
Mainous said: “Many infectious diseases are accompanied by increased inflammation. Most of the time the inflammation is concentrated or specific to where the infection is. Covid-19 is different because it creates inflammation in many places besides the airways, for example in the heart, brain and kidneys. High levels of inflammation can cause tissue damage.”
Importantly, the authors showed that the elevated risk of death from any cause associated with severe inflammation was again reduced by 51% if the patient was prescribed anti-inflammatory steroids after hospitalization .
These results mean that the severity of inflammation during Covid-19 hospitalization can predict the risk of subsequent serious health problems, including death, from ’long Covid’. They also imply that current recommendations for best practice may need to change to include more widespread prescribing of oral steroids to Covid-19 patients upon discharge.
Covid-19: a chronic disease?
Covid-19 should be viewed as a potentially chronic disease, the authors propose.
“When someone has a cold or even pneumonia, we usually think that the illness will be over once the patient recovers. This is different from a chronic disease, such as congestive heart failure or diabetes, which continue to affect patients after an acute episode. Similarly, we may need to start thinking about Covid-19 as having ongoing effects on many parts of the body after patients have recovered from the initial episode,” Mainous said.
"Once we recognize the importance of ’long Covid’ after apparent ’recovery’, we should focus on treatments to prevent subsequent problems such as strokes, brain dysfunction and, especially, premature death."
| In conclusion , hyperinflammation present with severe COVID-19 is associated with an increased risk of mortality after hospital discharge. Although suggestive, treatment with anti-inflammatory medications such as steroids at the time of hospital discharge is associated with a decreased risk of post-acute mortality from COVID-19. This suggests that treating inflammation may also benefit other post-acute sequelae such as long COVID. A reconceptualization of COVID-19 as both an acute and chronic condition may be helpful. |