In this cohort study that included 1,470 adults with chronic low back pain , patients treated by highly empathetic physicians reported significantly better, clinically relevant outcomes regarding pain, function, and health-related quality of life over 12 months. compared to patients treated by mildly empathetic doctors. Physician empathy was more strongly associated with favorable outcomes than nonpharmacological treatments, opioid therapy, and lumbar spine surgery.
These findings suggest that physician empathy is an important aspect of the physician-patient relationship and was associated with better outcomes among patients with chronic pain.
Empathy is an aspect of the doctor-patient relationship that may be particularly important in patients with chronic pain.
Design, environment and participants
This cohort study included adults enrolled in the National Pain Registry for Epidemiologic, Clinical, and Interventional Studies and the National Pain Research Registry. Study dates were April 1, 2016 to July 25, 2023, with up to 12 months of follow-up.
Exposure physician empathy was assessed with the measure of consultation and relational empathy and dichotomized to produce groups of highly empathetic physicians and mildly empathetic physicians .
Main results and measures
Main outcomes were patient-reported pain, function, and health-related quality of life (HRQoL) measured with a numerical rating scale for low back pain intensity, the Roland-Morris Disability Questionnaire for disability. Back-Related and Patient-Reported Outcomes Measurement Information System for HRQoL Deficits Related to Anxiety, Depression, Fatigue, Sleep Disturbances, and Pain Interference.
Data were collected at 5 quarterly meetings from registry enrollment to 12 months and analyzed with generalized estimating equations, including multivariable models to measure temporal trends and adjust for baseline and longitudinal covariates.
Results
Among the 1,470 patients , the mean (SD) age was 53.1 (13.2) years and 1,093 (74.4%) were women. Patients completed 5943 visits in which multivariable analyzes demonstrated that greater empathy for the physician was inversely associated with pain intensity (β = −0.014; 95% CI, −0.022 to −0.006; P < 0.001), disability related (β = −0.062; 95% CI, −0.085 to −0.040; P < 0.001) and HRQoL deficits on each measure (e.g., pain interference: β = −0.080; 95% CI %, −0.111 to −0.049; P < 0.001).
Consequently, compared with the mildly empathetic physician group, the highly empathetic physician group reported lower mean pain intensity (6.3; 95% CI, 6.1-6.5 vs. 6.7; 95% CI, 6.5-6.9; p < 0.001), less mean back pain. related disability (14.9; 95% CI, 14.2-15.6 vs. 16.8; 95% CI, 16.0-17.6; p < 0.001) and fewer HRQoL deficits on each measure (e.g., fatigue: 57.3; 95% CI, 56.1-58.5 vs. 60.4; 95% CI, 59.0-61.7; p < 0.001).
All differences between medical empathy groups were clinically relevant, with Cohen´s d statistics ranging from 0.21 for pain intensity to 0.30 for back-related disability, fatigue, and pain interference. .
Physician empathy was associated with more favorable outcomes than non-pharmacological treatments, opioid therapy, and lumbar spine surgery .
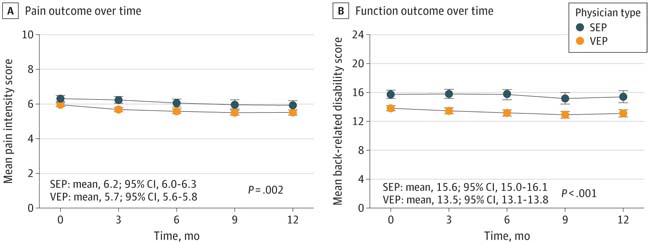
Figure: Pain and function outcomes over time . A, Measured with a numerical rating scale for the typical level of pain in the 7 days prior to each encounter, with scores ranging from 0 to 10. B, Measured with the Roland-Morris Disability Questionnaire, with scores ranging from 0 to 24. Higher scores on both assessments indicate worse outcomes in terms of pain and function. Physicians were classified as highly empathetic if their scores on the Consultation and Relational Empathy (CARE) measure were 30 or higher and as slightly empathetic if their scores were 29 or lower. Scores range from 10 to 50, with higher scores indicating greater empathy for the doctor. Mildly empathetic physicians made up approximately the lowest quartile on the CARE measure. Summary measures and P values are for the entire 12-month period adjusted for time and empathy × time interaction. Error bars represent 95% CIs. SEP indicates slightly empathetic doctor; VEP, very empathetic doctor.
Conclusions
In this cohort study of patients with chronic pain, physician empathy was associated with better longitudinal outcomes in pain, function, and HRQoL over 12 months, even in multivariable analyzes that controlled for the effects of time and a wide range of covariates including the current opioid use and lumbar spine surgery throughout the study.
The results of having a highly empathetic doctor were clinically relevant and better than those associated with non-pharmacological treatments, opioid therapy, and lumbar spine surgery. Physician empathy is an important aspect of the doctor-patient relationship among people with chronic pain. It appears that greater efforts are warranted to cultivate and enhance clinician empathy in this population.
















