Preamble
The guidelines summarize and evaluate the available evidence, with the aim of helping healthcare professionals propose the best management strategies for an individual patient with a given condition. The guidelines and their recommendations should facilitate the decision-making of health professionals in their daily practice. The guidelines, however, do not replace the patient’s relationship with their doctor. Final decisions regarding an individual patient should be made by the responsible healthcare professionals, based on what they consider most appropriate in the circumstances. These decisions are made in consultation with the patient and caregiver, as appropriate.
The guides are intended to be used by healthcare professionals. To ensure that all users have access to the latest recommendations, the European Society of Cardiology (ESC) makes its guidelines freely available. The ESC warns readers that technical language can be misinterpreted and declines any responsibility in this regard.
What’s new
The magnitude of the problem
The annual volume of major surgery worldwide is estimated to be more than 300 million patients (about 5% of the world’s population), representing a 34% increase between 2004 and 2012. Nearly 74% of These operations are carried out in countries that spend amounts on medical care. When applied to European Union countries, which had a total population of 448 million in 2020 (27 countries), this figure translates to a rough estimate of almost 22 million major procedures per year.
Nearly 85% of major operations are non-cardiac surgical procedures. In a recent report from the US National Inpatient Sample database , 18% had coronary artery disease (CAD), 4.7% had a history of stroke, and 7.7% had a Revised Cardiac Risk Index (RCRI) ≥3 (range 0–6) in 2012–13. These prevalence rates show a substantial increase compared to equivalent rates in 2008–09. In a large registry including 37,915 consecutive patients undergoing percutaneous coronary interventions (PCI) with drug-eluting stents (DES), NCS rates after PCI were 11%. and 24%, 1 and 3 years after PCI, respectively. The cutoff ages at which NCS was most likely to occur within 1 and 3 years of PCI were 62 and 73 years, respectively.
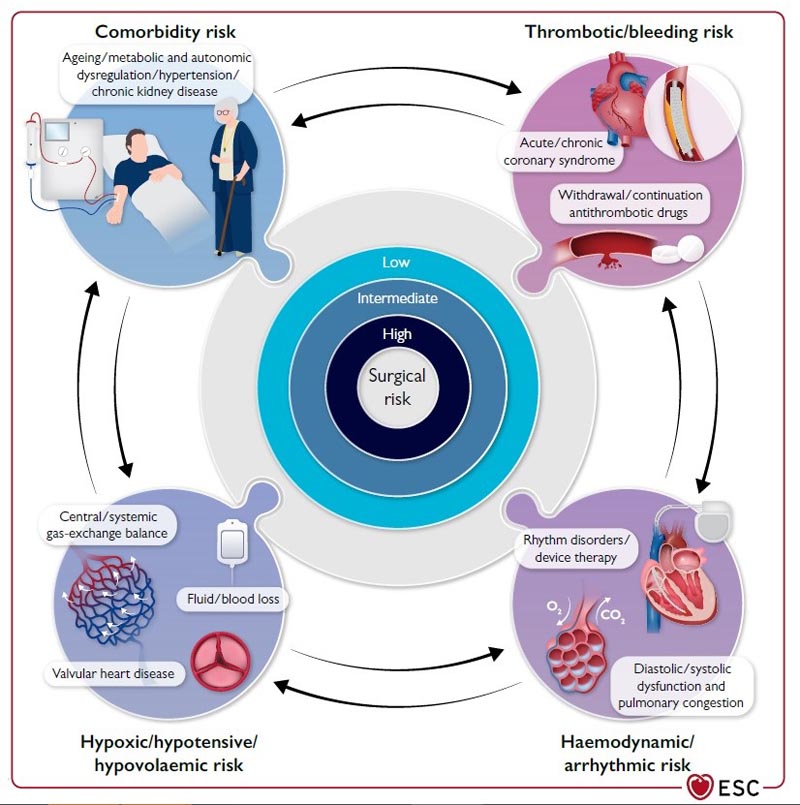
The prevalence of comorbidities, the clinical status of patients before surgery, and the urgency, magnitude, type, and duration of the surgical procedure determine the risk of perioperative complications. In a recent cohort study of 40,000 patients ≥45 years of age undergoing inpatient NCS, one in seven experienced a major cardiac or cerebrovascular complication at 30 days. Cardiovascular complications may occur particularly in patients with documented or asymptomatic coronary artery disease, left ventricle (LV), valvular heart disease (VHD), and arrhythmias, who undergo surgical procedures that are associated with prolonged hemodynamic and cardiac stress.
In the case of perioperative myocardial ischemia , three mechanisms are important: (i) mismatch between oxygen supply and demand in the context of coronary artery stenosis that can become flow-limiting due to perioperative hemodynamic fluctuations; (ii) acute coronary syndrome (ACS) due to stress-induced erosion or rupture of a vulnerable atherosclerotic plaque in combination with proinflammatory and hypercoagulable states induced by surgery, and hemodynamic discomfort resulting from fluid changes and anesthesia; and (iii) the risk of bleeding associated with surgery requiring discontinuation of antiplatelet therapies, which could lead to stent thrombosis in patients undergoing NCS after recent coronary stent placement.
Left ventricular dysfunction and arrhythmias can occur for various reasons at all ages. Because the prevalence of CAD, VHD, heart failure, and arrhythmias increases with age, perioperative mortality and CV morbidity are predominantly an issue in the adult population undergoing major NCS.
The 2022 ESC Guidelines on Cardiovascular Evaluation and Treatment of Patients Undergoing NCS focus on preoperative CV risk assessment and perioperative management of patients in whom cardiovascular disease (CVD) is a potential source of complications during NCS. .
A cardiac screening is recommended even in apparently healthy people over 65 years of age before intermediate- or high-risk non-cardiac surgery, according to the European Society of Cardiology (ESC) Guidelines on Cardiovascular Evaluation and Management of Patients Undergoing Non-cardiac Surgery published in European Heart Journal .
It is estimated that more than 300 million people undergo major surgery worldwide each year. Nearly 85% of major operations are non-cardiac procedures . In the European Union, it is estimated that at least 660,000 major cardiovascular complications occur annually due to non-cardiac surgeries. The document provides advice for the preoperative, operative, and postoperative care of patients undergoing noncardiac surgery. The goal is to prevent cardiovascular complications, including myocardial infarction, thrombosis (blood clots) in stents, heart rhythm disorders, pulmonary embolism, stroke and death.
The probability of cardiovascular complications depends on the patient’s characteristics as well as the type of surgery and whether it is elective or urgent. Surgeries are classified as low (less than 1%), intermediate (1-5%), and high (more than 5%) surgical risk based on the likelihood of heart attack, stroke, or death from cardiovascular disease within 30 days. For example, knee surgery is low risk, a kidney transplant is intermediate risk, and a lung transplant is high risk.
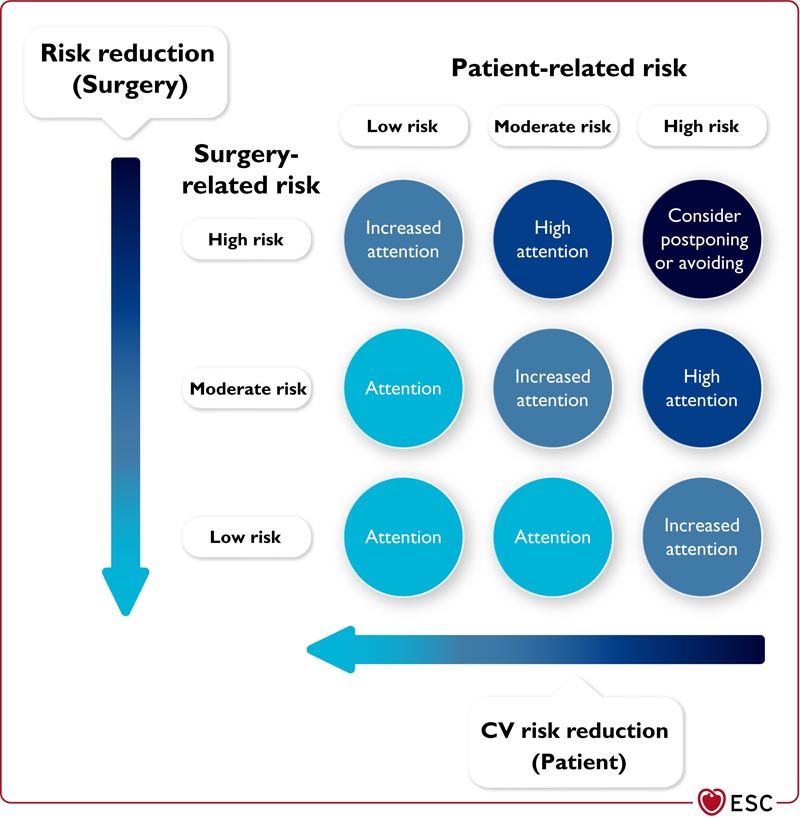
Figure: Total risk is an interaction of patient-related and surgery-related risk. Ideally, the total risk should be as close to the lower left corner as possible, choosing surgery/procedure/anesthesia/institution with the lowest possible risk along with efforts to mitigate the patient’s CV risk.
Professor Julinda Mehilli from Landshut-Achdorf Hospital, Landshut, Germany, said: "In patients aged 45 to 65 years without signs, symptoms or history of cardiovascular disease, an electrocardiogram (ECG) and troponin measurements should be considered before undiagnosed high-risk patients. -heart surgery."
The guideline outlines actions patients can take before and after surgery to reduce the likelihood of cardiovascular complications.
- It is recommended to stop smoking more than four weeks before surgery, as well as control high blood pressure, dyslipidemia and diabetes.
- Patients should be monitored for anemia, which should be treated before surgery.
- If patients are taking medications, particularly anticoagulants, their doctor should inform them whether they should stop or continue these medications.
Chair of the guidelines working group, Professor Sigrun Halvorsen from the University of Oslo Ulleval Hospital, Oslo, Norway, said: "It is very important that patients using anticoagulants receive detailed information on how to manage these medications before and after of surgery."
Risk assessment should encompass surgical and patient aspects so that individualized decisions can be made. The document states: “It is important that patients’ values and preferences regarding the benefits and risks of surgery are taken into consideration, and that patients are involved in decisions. “This is particularly important when it comes to decisions about whether or not to undergo elective surgery, the timing of surgery, and the choice of surgical and anesthetic techniques.”
The document provides personalized recommendations for patients with different cardiovascular conditions, kidney disease, diabetes, cancer, obesity and COVID-19. In general, after COVID-19, elective non-cardiac surgery should be postponed until complete recovery and optimization of coexisting conditions.
Existing heart disease increases the risk of perioperative cardiovascular complications, especially in elderly patients. All patients with coronary artery disease should receive a cardiac evaluation. The decision to pursue invasive diagnostic workup and revascularization with stents or bypass surgery before noncardiac surgery should be individualized based on symptoms and the presence of obstruction or narrowing of cardiac vessels.
Patients with symptomatic valvular heart disease , particularly those with aortic valve stenosis or mitral valve regurgitation, are at increased risk of perioperative complications, especially when undergoing intermediate- and high-risk noncardiac surgery.
Depending on the severity of aortic valve stenosis and the urgency and severity of planned noncardiac surgery, guidelines recommend surgical or transcatheter repair of the valve or balloon valvuloplasty as a bridge to repair.
People with severe mitral regurgitation often have heart failure, which doubles the risk of complications, particularly after intermediate- or high-risk noncardiac surgery. Percutaneous or surgical mitral valve repair should be considered before noncardiac surgery in addition to optimal guideline-indicated medical treatment.
Preoperative cardiac monitoring with ECG is also recommended in patients with arrhythmias who must continue taking their antiarrhythmic medication. Patients with a pacemaker or implantable cardioverter-defibrillator should have their device checked before surgery, if it has not been done recently.
After noncardiac surgery, particularly intermediate- and high-risk surgery, the most common cardiovascular complication is myocardial injury , which is associated with an increased risk of death within one month after surgery. Patients with heart disease are more likely to experience this complication and may require longer observation in intensive care than those without heart disease.
















