Eczema (atopic dermatitis) is common in babies and can be stressful for parents. An article in CMAJ ( Canadian Medical Association Journal ) describes practical tips for managing this condition.
"Atopic dermatitis affects 10 to 20 percent of Canadian babies. Recognizing atopic dermatitis, putting it into remission, and then maintaining control can be a challenge for both doctors and caregivers," says Dr. Derek Chu, assistant professor in the Division of Allergy and Immunology. at McMaster University and co-chair of the upcoming atopic dermatitis guidelines from the American Academy of Allergy, Asthma and Immunology and the American College of Allergy, Asthma and Immunology.
"We hope these five key messages for general and specialty care providers, as well as caregivers, will promote best practices for managing atopic dermatitis in babies. Atopic dermatitis affects more than just the skin and impacts the entire family , so optimal management of atopic dermatitis at this critical stage of a baby’s development is important."
Atopic dermatitis on the cheeks, outer limbs and trunk is common in babies, and classic eczema affecting behind the knees and in the creases of the elbows may not develop until later in childhood.
1. In infants, atopic dermatitis most commonly affects the cheeks, outer limbs, and trunk .
Classic flexural involvement may not develop until later in childhood. Other transient forms of dermatitis, including irritant dermatitis and seborrheic dermatitis, must be differentiated from atopic dermatitis.
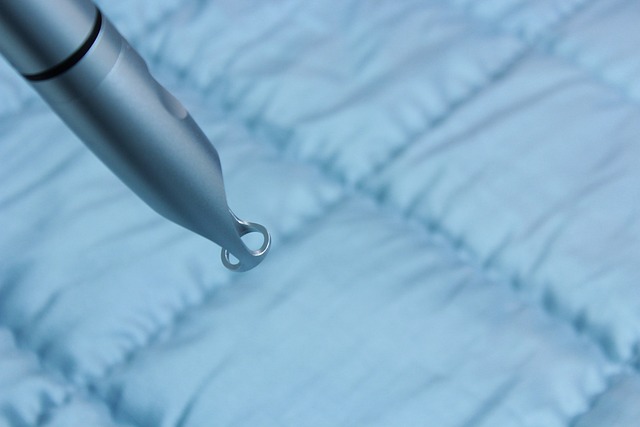
2. The best moisturizer is the one that caregivers and patients will use.
New evidence has shown that, applied twice daily and as needed, any kind of emollient (i.e., lotion, cream, gel, or ointment) can help control atopic dermatitis and prevent flare-ups.2 Emollient additives for skin care baths do not add benefits beyond direct hydration of the skin; however, emollients can be used as soap substitutes.3
3. Atopic dermatitis requires anti-inflammatory treatment
The lowest effective concentration of topical corticosteroids should be used . Applying the treatment once a day is almost as effective as applying it twice a day and can improve adherence and reduce adverse effects and costs. A reactive approach (anti-inflammatory treatment during a flare until the skin is clear) is appropriate for mild atopic dermatitis.
Recurrent or persistent cases may require a “gain control and maintain control” approach by inducing complete remission with the application of a moderate (e.g., betamethasone valerate 0.05%) or potent topical corticosteroid. (e.g., mometasone furoate 0.1%) to affected areas of the body (strong treatments should not be applied to the face), followed by approximately 3 months of treatment with moderate-strength corticosteroids or topical pimecrolimus for 2 consecutive days each week (for example, weekends).
4. Treatment of secondary bacterial infection should focus on the underlying skin inflammation .
Skin colonization or infection with Staphylococcal aureus is common, but evidence does not support the routine use of topical or oral antibiotics, which may contribute to antibiotic resistance. Oral antibiotics are only necessary if there are systemic infectious signs, such as fever.
5. Avoiding foods may not improve atopic dermatitis and risks promoting food allergy
Early introduction of allergenic foods to a baby can reduce the risk of developing food allergies. The Canadian Pediatric Society now recommends the introduction of allergenic foods around 6 months of age with continuation of breastfeeding until 2 years or older, if possible.
Summary to remember
|