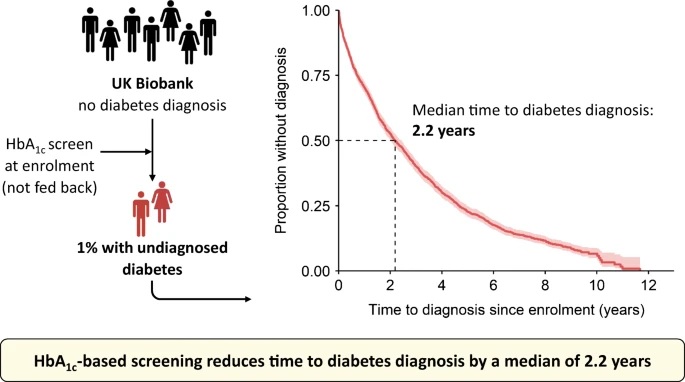
Summary Objectives/hypotheses Screening programs can detect cases of undiagnosed diabetes earlier than symptomatic or incidental diagnosis. However, the improvement in time to diagnosis achieved by screening programs compared with usual clinical care is unclear. Our aim was to use the UK Biobank population-based study to provide the first population-based estimate of the reduction in time to diabetes diagnosis that could be achieved by HbA1c-based screening in middle-aged adults. Methods We studied UK Biobank participants aged 40-70 years with HbA1c measured at enrollment (but not fed back to participants/clinicians) and linked primary and secondary healthcare data (n=179,923) and identified to those with a diagnosis of pre-existing diabetes (n= 13,077, 7.3%). Among the remaining participants (n=166,846) without a diagnosis of diabetes, we used an elevated HbA1c level (≥48 mmol/mol [≥6.5%]) to identify those with undiagnosed diabetes. For this group, we used Kaplan-Meier analysis to evaluate the time between HbA1c measurement and subsequent clinical diagnosis of diabetes up to 10 years, and Cox regression to identify clinical factors associated with delay in diabetes diagnosis. diabetes. Results In total, 1.0% (1,703/166,846) of participants without a diagnosis of diabetes had undiagnosed diabetes based on calibrated HbA1c levels at UK Biobank enrollment, with a median HbA1c level of 51. 3 mmol/mol (IQR 49.1–57.2) (6.8% [6.6 –7.4]). These participants represented an additional 13.0% of diabetes cases in the study population relative to the 13,077 participants diagnosed with diabetes. The median time to clinical diagnosis for people with undiagnosed diabetes was 2.2 years, with a median HbA1c at clinical diagnosis of 58.2 mmol/mol (IQR 51.0–80.0) (7.5% [6.8–9.5]). Female participants with lower HbA1c and BMI measurements at enrollment experienced the longest delay to clinical diagnosis. Conclusions/interpretation Our population-based study shows that HbA1c screening in adults aged 40 to 70 years can reduce time to diabetes diagnosis by a median of 2.2 years compared to usual clinical care. The findings support the use of HbA1c screening to reduce the time people live with undiagnosed diabetes. |
Comments
The study suggests that at least a quarter of a million cases would be found through population screening, and probably many more
Using a standard diabetes test to screen all UK adults aged 40 to 70 would find undiagnosed cases of type 2 diabetes more than two years earlier and help those people start treatment at a much earlier stage. early in his condition. The study is published in Diabetologia (the journal of the European Association for the Study of Diabetes [EASD]) and is led by Dr. Katie Young, Dr. John Dennis and Dr. Nicholas Thomas, from the University of Exeter, United Kingdom, and colleagues.
This is the first study to use real-world clinical data (from the UK Biobank) to determine how many diabetes diagnoses would be brought forward in a large population cohort by implementing a diabetes screening programme. The authors believe that the potential for finding previously undiagnosed cases could be even greater than their study suggests, as the UK Biobank population is healthier than the general population, and ethnic minorities such as blacks and whites South Asians are underrepresented in the UK Biobank cohort and have higher rates of diabetes.
The authors studied UK Biobank participants aged 40 to 70 years who had their HbA1c (glycated hemoglobin) measured at enrollment. HbA1c reflects a person’s blood sugar control over the past 2 to 3 months, and is more widely used and convenient than the oral glucose tolerance test (another commonly used method). HbA1c is expressed as an absolute value (mmol/mol) or as a percentage, with a cutoff of 48 mmol/mol or higher (6.5% or higher) often used to diagnose diabetes.
Participants’ HbA1c results were not reported to the participants or their physicians. The researchers then analyzed the 179,923 participants with linked healthcare data and identified those with a pre-existing diabetes diagnosis (n = 13,077, 7.3%). Among the remaining participants (n=166,846) without a diagnosis of diabetes, 1.0% (1,703) had undiagnosed diabetes based on their HbA1c at enrollment. These participants added an additional 13% of cases to the 13,077 participants diagnosed with diabetes.
There are approximately 25 million adults aged 40 to 70 years living in the UK today without a diagnosis of diabetes, so the authors’ estimate of 1.0% with undiagnosed diabetes suggests that up to 250,000 adults in this age group have undiagnosed diabetes that could be detected by HbA1c-based screening. However, this is likely an underestimate for the reasons described above and below. Diabetes UK estimates that there are 850,000 people living with undiagnosed diabetes in the UK.
In this study, the median time to clinical diagnosis for people with undiagnosed diabetes was 2.2 years , with a median HbA1c at clinical diagnosis of 58.2 mmol/mol (7.5%). . At 10 years of follow-up, 88% of those 1,703 undiagnosed cases had received a clinical diagnosis.
Female participants with lower HbA1c and BMI measurements at enrollment experienced the greatest delay in clinical diagnosis; This suggests that physicians are currently more likely to screen men or people with obesity and less likely to screen women or people with a BMI below the obese range (less than 30 kg/m2).
Given the known associations between non-white ethnicity and greater social deprivation and increased risk of diabetes, the authors say the prevalence of undiagnosed diabetes in this age group in the broader population is likely to be higher than that seen in UK Biobank (1.0%); Studies in other UK cohorts give estimates of 2.8 to 4.5%.
Furthermore, since UK Biobank participants are likely to be more health conscious than average, like volunteers in other research studies, they may have more frequent doctor’s appointments and therefore be diagnosed them with diabetes before. This suggests that screening efforts in the "normal" general population of adults aged 40 to 70 years could identify even more cases of undiagnosed diabetes and reduce the time to diagnosis even more than the 2.2 years observed in this study.
However, they also add that increases in opportunistic diabetes testing during and after the study period may mean that any screening initiative implemented today would provide less substantial benefits than the 2.2-year improvement seen in this study, supported by the reduction in time to diagnosis seen in the study between recruitment in 2008 and recruitment in 2010. However, other issues have hampered diabetes testing recently, including the COVID-19 pandemic which resulted in fewer HbA1c testing and delays in diagnosing type 2 diabetes. Healthcare spending in the UK is under intense pressure as economic circumstances worsen. The authors say all of this means that “diabetes screening initiatives could be more important than ever to avoid long delays in diagnosis.”
The authors also highlight that unless ways to identify people at risk for diabetes (diabetes risk scores) are improved, population-based screening with HbA1c is the only way to reliably identify non-diabetes. diagnosed. Currently in England, the NHS Health Check for adults aged 40 to 74 includes diabetes screening for those at "high risk" of diabetes according to the Leicester Risk Score .
However, as highlighted in this study, these risk scores do not identify all patients with undiagnosed diabetes and do not work as well in those without obesity, so there is a need for greater awareness among healthcare professionals. health on the importance of type 2 diabetes controls in people without obesity . On this, they say: "However, the cost-effectiveness of this population-wide screening test for older adults deserves further evaluation and will vary depending on current HbA1c testing levels in the underlying population."
The authors conclude: "Our study provides the first population-based estimate of the impact of HbA1c-based screening on reducing time to diabetes diagnosis. In UK Biobank, 1.0% of people aged 40 to 70 years had undiagnosed diabetes, and HbA1c screening at the population level could have reduced the time to diabetes diagnosis in this group by a median of 2.2 years. Earlier diagnosis would allow for earlier intervention with the potential to reduce the risk of diabetes complications, but this requires further evaluation.”
















