Among 35,864 UK residents , each one-year increase in retinal age, assessed by changes in retinal microvasculature, was associated with a 10% increased risk of incident renal failure over 11 years of follow-up.
There is a pressing need to identify early predictive biomarkers of renal failure, given its associated substantial morbidity and mortality. Biomarkers of aging have been associated with kidney failure, but their clinical application has been challenging.
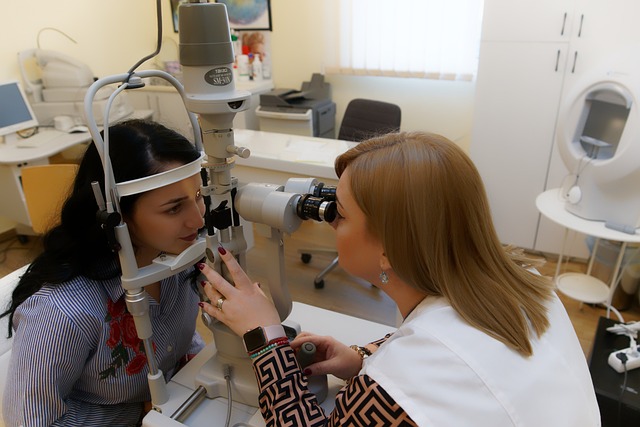
In this study published in the American Journal of Kidney Diseases (AJKD), retinal age difference (retinal-predicted age minus chronological age), a clinically validated, artificial intelligence-powered biomarker of aging based on images of the retina, was associated with future risk of kidney failure among UK residents.
This non-invasive biomarker of aging may show promise in aiding in the identification of individuals at high risk for kidney failure.

Justification and objective
The incidence of end-stage kidney disease (ESKD) is known to increase with age. We have previously developed and validated retinal age based on fundus images used as a biomarker of aging. However, the association of retinal age with ESKD is unclear. We investigated the association of the difference between retinal age and chronological age, retinal age gap , and future risk of ESKD.
Study design
Prospective cohort study.
Setting and participants
11,052 UK Biobank study participants without any reported disease to characterize retinal age in a deep learning algorithm. An additional 35,864 participants with retinal imaging and without ESKD were followed to evaluate the association between retinal age difference and ESKD risk.
Exposure
Retinal age gap defined as the difference between model-based retinal age and chronological age.
Evolution
Incident kidney disease.
Analytical approach
A deep learning prediction model used to characterize retinal age based on retinal images and chronological age. Cox proportional hazards regression models to investigate the association of retinal age difference with incident ESRD.
Results
After a median follow-up of 11 years (interquartile range [IQR]: 10·89-11·14), 115 (0·32%) participants were diagnosed with ESKD.
Each one-year increase in retinal age difference was independently associated with a 10% increase in the risk of ESRD incidence (hazard ratio [HR] = 1·10, confidence interval [CI] 95%: 1·03-1·17, P = 0·003).
Participants with retinal age gaps in the fourth quartile had a significantly increased risk of incident ESKD compared with those in the first quartile (HR = 2.77, 95% CI: 1.29-5.93, P = 0.009).
Limitations
Limited generalizability due to the composition of participants in the UK Biobank study.
Conclusion
Retinal age gap was significantly associated with incident ESKD and may be a promising non-invasive biomarker for incident ESKD.