The electrocardiogram (ECG) treadmill stress test , also known as a stress test , is one of the most familiar tests in medicine. While exercise testing typically focuses on diagnosing coronary artery disease, a recent Mayo Clinic study finds that abnormalities on exercise testing, such as low functional aerobic capacity , predicted non-cardiovascular causes of death, such as cancer, in addition to deaths related to cardiovascular diseases. These new findings are published in Mayo Clinic Proceedings .
Stress testing is noninvasive, readily available, and provides important diagnostic information. In addition to the ECG itself, the test produces data on functional aerobic capacity, heart rate recovery, and chronotropic index, the standardized measure of heart rate during exercise that reflects age, resting heart rate, and physical fitness. .
"In our exercise testing cohort, noncardiovascular deaths were seen more frequently than cardiovascular deaths," says Thomas Allison, Ph.D., MPH, director of the Mayo Clinic Integrated Stress Testing Center and senior author. of the study. "Although this was a cardiac stress test, we found that cancer was the leading cause of death, at 38%, while only 19% of deaths were cardiovascular. The results of the exercise tests included low exercise, low maximum heart rate, and slow recovery of heart rate after stress testing were associated with increased mortality."
The study looked at 13,382 patients who did not have cardiovascular problems or other serious illnesses and who had completed exercise testing at Mayo Clinic between 1993 and 2010, and then were followed closely for an average period of 12.7 years.
The findings suggest that clinicians should focus not only on ECG results but also on exercise testing data, such as low functional aerobic capacity, low chronotropic index, and abnormal heart rate recovery. Patients should be encouraged to increase their physical activity if these results are atypical, even if the ECG results do not show any significant cardiovascular risk, says Dr. Allison.
Treadmill stress testing is a commonly available, noninvasive, and relatively cost-effective risk stratification tool that can provide important diagnostic and prognostic information. Electrocardiogram (ECG) interpretation is an important part of exercise testing, but important additional prognostic value can be gained from parameters such as functional aerobic capacity (FAC), heart rate recovery, and chronotropic index.
A common outcome in large studies showing the prognostic significance of stress test results is all-cause mortality, including classic studies that first established exercise capacity as an important prognostic factor.
This is probably because total mortality is readily available and uncontroversial. Because stress testing is a procedure primarily focused on the diagnosis of coronary artery disease, and because cardiovascular (CV) disease is the leading cause of death in the United States, there is an unspoken assumption that mortality from all causes will be a surrogate for CV mortality. However, in cohorts in which significant baseline CV disease is excluded, this assumption may not be correct. This implies that stress testing can also predict non-CV death . However, the relationship of stress test parameters with non-CV death has not been fully described.
The purpose of the present study was to: (1) determine the distribution of causes of death in a primary prevention cohort referred for stress testing; and (2) determine the role of stress test parameters including low FAC, abnormal heart rate recovery, chronotropic incompetence, and abnormal stress ECG in predicting non-CV death in a population referred for stress testing without disease. Initial CV.
Aim
To identify specific causes of death and determine the prevalence of non-cardiovascular (non-CV) deaths in a population referred for stress testing while testing whether stress test parameters predict non-CV and CV deaths.
Patients and methods
Nonimaging stress tests were reviewed in patients aged 30 to 79 years from September 1993 to December 2010. Patients with baseline cardiovascular disease and non-Minnesota residents were excluded. Mortality through January 2016 was obtained from Mayo Clinic records and the Minnesota Death Index.
Abnormalities on exercise testing included low functional aerobic capacity (FAC) (i.e., less than 80%), heart rate recovery (i.e., less than 13 beats/min), low chronotropic index (i.e., less of 0.8) and abnormal stress electrocardiogram (ECG) of greater than or equal to 1.0 mm of ST depression or elevation. We also combined these four abnormalities into a composite exercise test score (EX_SCORE).
Statistical analyzes consisted of Cox regression adjusted for age, sex, diabetes, hypertension, obesity, current and past smoking, and heart rate-lowering drugs.
Results
The study identified 13,382 patients (women: n=4,736, 35.4%, 50.5±10.5 years of age). During 12.7±5.0 years of follow-up, there were 849 deaths (6.3%); Of these, 162 (19.1%) were from CV; 687 (80.9%) were not CV.
Non-CV death hazard ratios were significant for low functional aerobic capacity (HR, 1.42; 95% CI, 1.19 to 1.69; P < 0.0001), abnormal heart rate recovery (HR, 1.36; 95% CI, 1.15-1.61; P < .0033) and a low chronotropic index (HR, 1.49; 95% CI, 1.26-1.77 ; p < 0.0001), while abnormal stress ECG was not significant.
All stress test abnormalities, including EX_SCORE, were more strongly associated with CV death than non-CV death, except abnormal stress ECG.
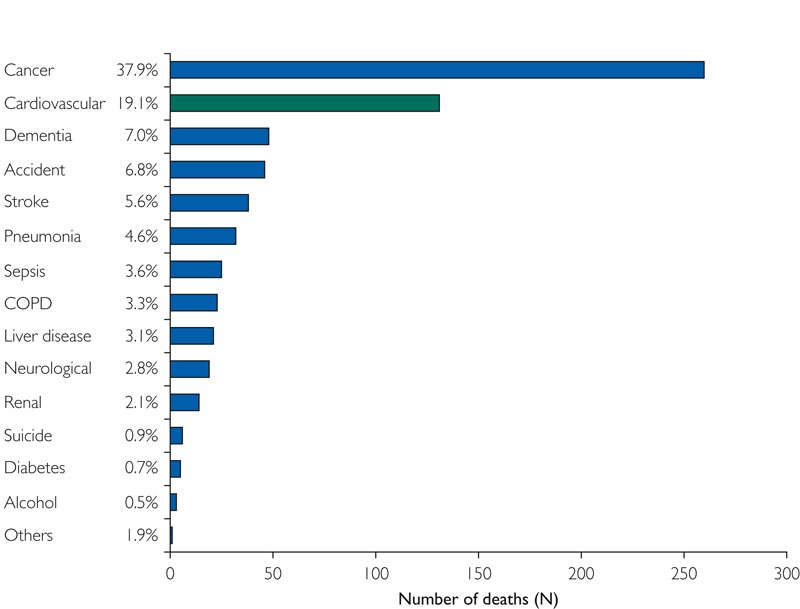
Figure : Primary causes of death. COPD = chronic obstructive pulmonary disease.
Discussion
The main new finding of this work is that non-CV deaths predominate in a primary prevention cohort in the absence of significant baseline CV disease. We believe our study is the first to show all primary causes of death in a stress-tested cohort. Furthermore, we demonstrate that exercise test parameters (including low aerobic functional capacity (FAC), abnormal heart rate recovery, and low chronotropic index, as well as a composite EX_SCORE combining the four exercise test abnormalities) exercise) predict not only CV death but also non-CV death, and that the ability to predict non-CV death is not solely due to death from cancer .
Ischemic changes on stress ECG were the weakest parameter for predicting death. ST change was found to be a significant predictor only of CV death , but not non-CV death , validating the importance of a complete interpretation of the stress test in determining prognosis.
Patients who died were older and had more hypertension, diabetes, and low FAC compared to those who survived. Patients who experienced CV death also had a higher prevalence of low aerobic functional capacity (FAC), low chronotropic index, and abnormal heart rate recovery, and lower composite EX_SCORE than patients who died from non-CV death. All stress test abnormalities, except abnormal stress ECG, were more powerful in predicting CV than non-CV death . In accordance with the recommendations provided by the American Heart Association guidelines , we are reinforcing the considerable prognostic value of the stress test that is largely independent of the electrocardiogram.
This value is not only related to CV death but also to many non-CV deaths.
Although the relationship between exercise capacity and non-CV mortality seems logical, it is less clear why abnormal heart rate responses also predict non-CV death. On the one hand, they may simply serve as secondary measures of reduced or poor exercise capacity. On the other hand, abnormal heart rate responses may indicate that autonomic impairment is an early marker of many chronic diseases, both CV and non-CV.
Conclusion In our exercise testing cohort without any significant baseline CV disease, non-CV deaths were more frequently observed . This is probably true in other stress testing studies that use similar primary prevention cohorts and present total mortality as an outcome variable. We believe that the data presented here show that stress test abnormalities not only predict CV death but also predict non-CV deaths. Specifically, low aerobic functional capacity (FAC), low chronotropic index, and abnormal heart rate recovery are associated with increased non-CV mortality after adjustment for age, sex, diabetes, hypertension, current and previous smoking, obesity, and use of drugs to reduce heart rate. These results were not significantly different after adjusting for possible underrepresentation of CV deaths by excluding contributory CV deaths and for premorbidity by excluding up to 7 years of early deaths. We suggest that clinicians also focus on non-ECG prognostic parameters when interpreting stress testing, rather than analyzing ECG parameters alone, and recognize that stress test results also predict non-CV death. Patients should be encouraged to increase physical activity if these prognostic parameters are abnormal, even in the absence of substantial CV risk based on ECG. |
Final message
Non-cardiovascular deaths predominated in this primary prevention cohort. Stress test abnormalities not only predicted CV death but also non-CV death.
















