clinical question
How can I improve outcomes for older adults with chronic kidney disease (CKD)?
Background
Chronic kidney disease is associated with substantial morbidity and health care costs. Strategies and tools to predict and delay progression to end-stage renal disease (ESRD) are vital, especially for patients with clinical frailty or comorbidities.
Evidence
|
Risk factor management
Control of blood pressure, lipid levels, and blood glucose levels are cornerstones of CKD treatment. Hypertension Canada recommends a target blood pressure of less than 130/80 mm Hg in patients with diabetes and less than 120/80 mm Hg in others.
Kidney disease : The 2021 Guidelines for Improving Global Outcomes (KDIGO) recommend intensive blood pressure reduction with or without diabetes; However, Hypertension Canada and KDIGO recognize the limitations of the evidence for lowering blood pressure in older adults and patients with substantial frailty or propensity to fall require an individualized approach. An example of adverse effects due to aggressive blood pressure lowering in older patients is postural hypotension which can lead to falls and trauma.
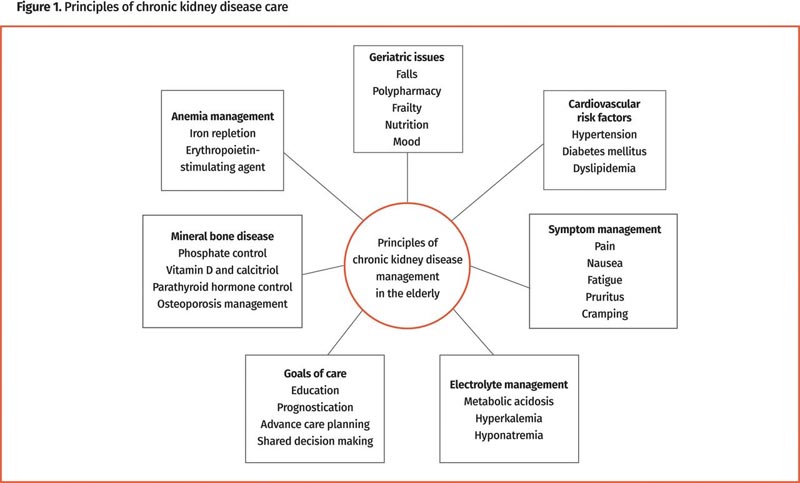
Figure: Principles of chronic kidney disease care
Likewise, it is necessary to individualize glycemic control . Canadian guidelines recommend that hemoglobin A 1c goals depend on frailty or cognition, focusing on avoiding extreme blood glucose levels.
The effect of lipid management is attenuated in those over 85 years of age. Reducing statin doses should be considered in older people with CKD and patients should be monitored for myopathy. It may be prudent to defer statin treatment in frail patients with poor nutrition and risk of sarcopenia.
Other management
Anemia is common in CKD and is often related to a relative deficiency of erythropoietin . Symptoms can be magnified in elderly patients and affect quality of life. Anemia with CKD is associated with increased cardiovascular events, hospitalizations, transfusions, and death.
Although ferritin levels are often elevated in patients with CKD, iron deficiency is still possible: KDIGO recommends an intravenous iron test for patients with transferrin saturation less than 30% and ferritin levels less than 500 μg/L despite of oral supplementation.
According to the Canadian Society of Nephrology guidelines, an erythropoietin-stimulating agent should be initiated when the hemoglobin level is between 90 and 100 g/L, with a target range of 100 to 110 g/L. Dosing and monitoring should be managed by nephrologists.
There is a high risk of fragility fractures in patients with CKD. Bone densitometry scans can be difficult to interpret in CKD, but the most recent guidelines recommend using them to follow the effects of treatment. As CKD progresses, the ability to hydroxylate 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D decreases and calcitriol supplementation is often required.
Bicarbonate loss and decreased acid excretion resulting in metabolic acidosis can be found in people with CKD . Chronic metabolic acidosis can contribute to osteopenia, muscle catabolism, and systemic inflammation , all of which contribute to frailty. There is increased mortality associated with bicarbonate levels less than 22 mmol/L; KDIGO recommends starting oral bicarbonate treatment when serum levels fall below this threshold.
Patients with end-stage renal disease (ESRD) may experience uremic symptoms including fatigue, decreased appetite, metallic taste (dysgeusia), dyspnea, edema, and cognitive changes. Although dialysis can provide survival and improve symptoms, these benefits are often modest in frail patients and may result in reduced quality of life and independence. Elderly patients undergoing dialysis experience a substantial symptom burden, with an average of 5 to 6 symptoms and the predominant one being fatigue. Home modalities, such as peritoneal dialysis, may be better tolerated and can be provided with the help of home care programs.
Implementation
Patients with a KFRE score greater than 5% over 5 years should be referred to a nephrologist , and those at increased risk for advanced progressive kidney disease (KFRE >10%) should be treated in a multi-care renal clinic by a team that includes nurses, pharmacists, dieticians, social workers and physicians. Treatment of elderly patients should incorporate geriatric competencies, including assessment of frailty, cognitive impairment, and multiple medications.
Goals of care planning
As kidney function declines, it becomes imperative to discuss future planning and goals related to ESKD and renal replacement therapy. It is important that the patient and her family participate in shared decision making with providers and are informed about the possible benefits, harms, or consequences of renal replacement therapy.
Conservative renal care without dialysis may be a good option in patients with comorbidities and frailty. This focuses on alleviating symptoms and avoiding invasive therapies that provide little benefit in terms of symptoms and survival. Tools such as the Clinical Frailty Scale can be useful in identifying patients who would benefit from conservative treatment.
Fostering partnerships between family medicine, nephrology, geriatrics, and palliative medicine would help establish a holistic approach to care and ensure that patients’ goals and values are incorporated into CKD treatment.
Grades
Geriatric Gems are produced in association with the Canadian Geriatrics Society Journal of CME, a free peer-reviewed journal published by the Canadian Geriatrics Society (http://www.geriatricsjournal.ca). The articles summarize evidence from review articles published in the Canadian Geriatrics Society Journal of CME and offer practical approaches for family physicians caring for older patients.















