Highlights
|
Summary
The accumulated literature linking stress to negative health outcomes, including cardiovascular diseases (CVD), is widely reported but poorly defined. Stress is associated with an increased risk of hypertension, acute myocardial infarction, arrhythmogenesis, and heart failure. Stress mediates its effect through neuronal, endocrine, autonomic and immunological processes directly and indirectly by modifying lifestyle behaviors that promote CVD progression.
Stress occurs when an individual perceives that internal or external demands exceed the capacity for adaptive response. Psychological stress is increasingly recognized in the atrial fibrillation (AF) population, although the pathophysiology remains unclear.
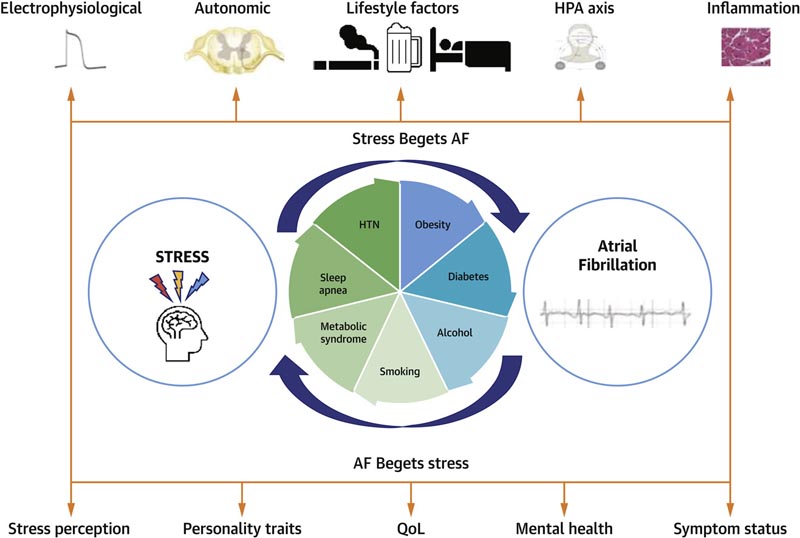
There appears to be a bidirectional relationship between AF and stress with a complex interaction between the two entities. Stress modulates the autonomic nervous and immune systems, key drivers in the initiation and potentiation of AF. AF leads to increased anxiety, psychological distress, and suicidal ideation.
Recently, lifestyle modification has become the fourth pillar of AF treatment, with stress reduction being a possible reversible risk factor and a future target for intervention. This review examines proposed mechanisms linking AF and stress and explores stress reduction as an adjunct to the AF management armamentarium.
Comments
Stress has been linked to poor health outcomes, although the exact mechanism remains poorly defined. Psychological stress is recognized as a contributing factor to atrial fibrillation (AFib), both in the onset and progression of AFib. The diagnosis of AFib is often associated with increased anxiety, psychological distress, and suicidal ideation.
In a review article published in JACC: Clinical Electrophysiology , possible mechanisms linking stress and atrial fibrillation and the possible use of stress reduction in the treatment of atrial fibrillation are explored.
Atrial fibrillation is an irregular and often rapid heart rhythm that can cause blood clots to form in the heart. People diagnosed with AFib have an increased risk of stroke, heart failure, and other heart-related complications. AFib is the most common arrhythmia worldwide.
There is significant global variation in people who report psychological stress, but on average 1 in 3 people experience it.
The authors define stress “as the perception of internal or external demands that exceed a person’s capacity for an adaptive response.” Reported stress levels have increased annually with the COVID-19 pandemic, leading to an even greater increase in self-reported psychological distress.
"We are seeing that psychological stress and even negative emotions are associated with the onset and enhancement of atrial fibrillation ," said the study’s senior author, Peter Kistler, MBBS, PhD, director of clinical electrophysiology research at Baker Heart and Heart Clinic. Diabetes Institute and director of electrophysiology at Alfred Hospital in Melbourne, Australia.
“By recognizing stress as a potentially modifiable risk factor in these patients, it builds on a more holistic approach to the management of atrial fibrillation. As such, targeted stress reduction may improve symptom perception and outcomes for patients with atrial fibrillation.”
The researchers examined studies on the role of stress in atrial fibrillation, as well as modification of traditional risk factors for atrial fibrillation, such as diet, alcohol cessation, and exercise.
The review also focuses on the bidirectional nature of the relationship between atrial fibrillation and stress. The study authors analyzed the role of acute and chronic stress in the induction of AFib; the role that stress plays in the physiological change of the heart; gender differences in response to stress; as well as how to measure stress, which is often subjective and self-reported.
“We also need to better consider the bidirectional nature of stress and atrial fibrillation. More and more studies show that it works both ways,” Kistler said. “Stress begets AFib and AFib begets stress. When treating patients with atrial fibrillation, doctors tend to focus on the physical symptoms of atrial fibrillation and do not fully consider the initial and evolving mental health consequences of having a heart rhythm disorder.”
According to the review, stress and negative emotions are often accompanied by modifiable risk factors. For example, people who experience chronic stress often report increased smoking, alcohol use, weight gain, and physical inactivity. Risk factors contribute to worsening atrial fibrillation symptoms in patients. Possible treatment options to reduce stress as part of AF management included further studies of antianxiety and antidepressant therapy, mindfulness-based stress reduction, and yoga.
“Physicians must recognize and address the psychosocial implications of an atrial fibrillation diagnosis by providing patient education and reassurance alongside conventional interventions to reduce symptoms and improve quality of life,” Kistler said. “When considering the impact of stress on illness perception, recognizing and mitigating stress can reduce symptoms and distress, improve resilience, and modify health behaviors to improve outcomes.”
The authors conclude that more research is needed to establish standardized methods for detecting and quantifying stress, while randomized trials are needed to better evaluate the impact of stress reduction on the management of atrial fibrillation.