Importance
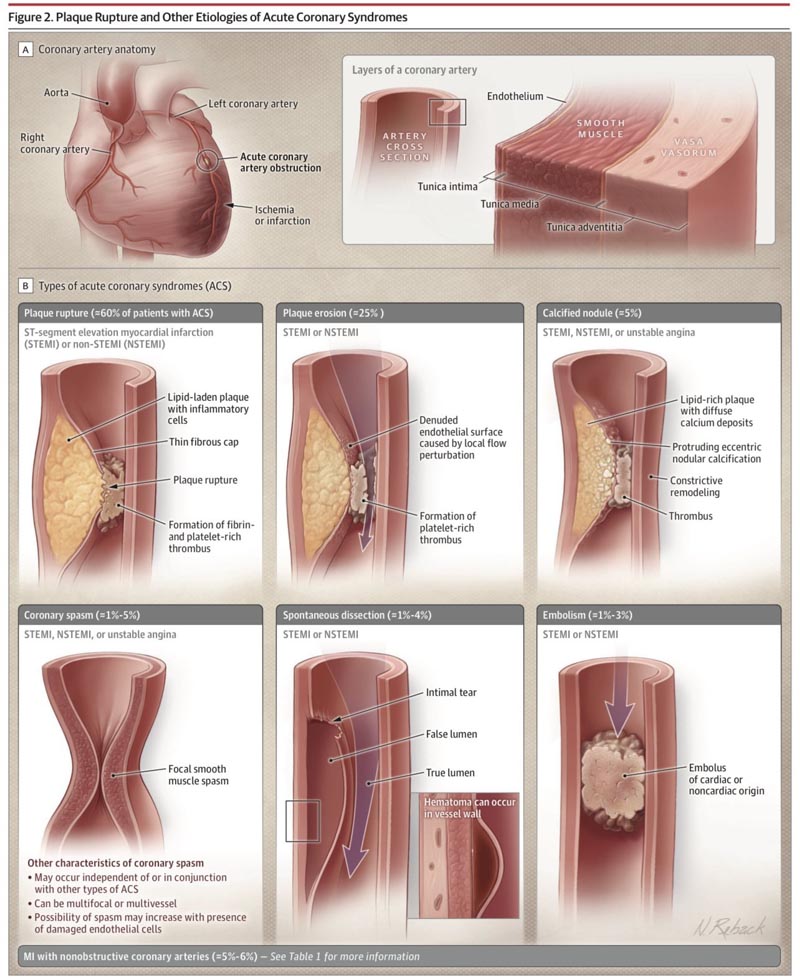
Acute coronary syndromes (ACS) are characterized by a sudden reduction in blood supply to the heart and include ST-segment elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), and unstable angina.
Each year, it is estimated that more than 7 million people worldwide are diagnosed with ACS, including more than 1 million hospitalized patients in the US.
Observations
Chest discomfort at rest is the most common presenting symptom of ACS, affecting approximately 79% of men and 74% of women with ACS, although approximately 40% of men and 48% of women experience nonspecific symptoms , such as dyspnea, either alone or, more commonly, in combination with chest pain.
For patients presenting with possible ACS, electrocardiography should be performed immediately (within 10 minutes of presentation) and can distinguish between STEMI and non-ST segment elevation ACS (NSTE-ACS).
ST-segment elevation infarction (STEMI) is caused by complete occlusion of the coronary artery and accounts for approximately 30% of ACS.
Acute coronary syndrome (ACS) without significant elevation of the ST segment on electrocardiography, called NSTE-ACS, represent approximately 70% of ACS, are caused by partial or intermittent occlusion of the artery and are associated with ST segment depressions (approximately 31%), T-wave inversions (approximately 12%), ST-segment depressions combined with T-wave inversions (16%), or none (approximately 41%).
When electrocardiography suggests STEMI, rapid reperfusion with primary percutaneous coronary intervention (PCI) within 120 minutes reduces mortality from 9% to 7%.
If PCI is not possible within 120 minutes, fibrinolytic therapy with alteplase, reteplase, or tenecteplase should be administered at full dose for patients younger than 75 years without contraindications and at half dose for patients 75 years or older (or streptokinase at full dose if cost), followed by transfer to a facility aiming for PCI within the next 24 hours.
High-sensitivity troponin measurements are the preferred test to evaluate NSTEMI.
In high-risk patients with NSTE-ACS and no contraindications, rapid invasive coronary angiography and percutaneous or surgical revascularization within 24 to 48 hours is associated with a reduction in death from 6.5% to ??4.9%.
Conclusions and relevance
|















