Advances in the treatment of chronic diseases have led to a steady increase in the number of pregnancies complicated by maternal congenital heart disease (CHD), rheumatic heart disease, cardiomyopathy, and arrhythmias. These conditions may predispose women and their children to adverse events during pregnancy and the postpartum period.
The placenta is responsible for maintaining the health of the fetus and abnormalities are associated with adverse fetal outcomes. Placental development is also affected by maternal conditions, and placental pathology has been linked to both active maternal disease and risk of future health problems.
While there are associations between placental health and maternal obesity, diabetes, and hypertension, there are very few studies examining the impact of other maternal cardiovascular diseases (CVDs) on the placenta. Such information could improve our understanding of the pathophysiological mechanisms responsible for adverse fetal outcomes in women with CVD during pregnancy and, in turn, could inform patient counseling and guide surveillance during pregnancy.
In this study, we sought to describe the pathological profile of placentas from pregnancies in women with CVD and to search for associations between types of maternal CVD and different placental pathologies.
Villitis of unknown etiology (VUE), also known as chronic villitis, is a placental lesion. It is an inflammatory condition that involves the chorionic villi (placental villi). Furthermore, it is a recurrent condition and may be associated with intrauterine growth restriction (IUGR). IUGR involves poor fetal growth, stillbirth, spontaneous abortion, and premature birth.12 It recurs in approximately 1/3 of subsequent pregnancies.
Background
The incidence of pregnancy in women with cardiovascular disease (CVD) has increased, but little is known about placental pathology in these women.
Goals
The objectives of this study were to describe placental pathology in pregnancies complicated by maternal CVD and to compare findings between categories of maternal CVD.
Methods
A single-center retrospective study was performed. Pathology reports of 264 placentas from pregnancies complicated by maternal CVD were reviewed for prespecified pathological findings that were then compared with maternal characteristics.
Results
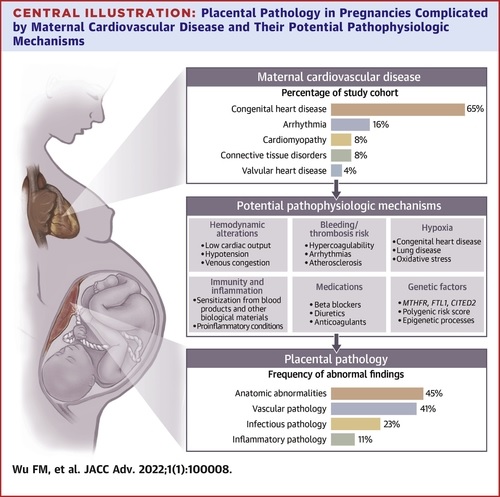
Placentas were from pregnancies associated with maternal congenital heart disease (n = 171), arrhythmia (n = 43), cardiomyopathy (n = 20), connective tissue disease (n = 20), and valvular heart disease (n = 10).
- The median maternal age at the time of delivery was 32 years (range: 19-49).
- The median gestational age at delivery was 39 weeks (range: 25-41).
Placental pathology was identified in 75% (199/264) of placentas. Anatomical pathology, mainly small placenta by weight, was present in 45% (119/264) of placentas.
Vascular pathology, primarily maternal vascular malperfusion or fetal vascular malperfusion, was observed in 41% (107/264) of placentas.
Acute chorioamnionitis and vylitis of unknown etiology (VUE) were observed in 23% (61/264) and 11% (28/264) of placentas, respectively. The prevalence of VUE differed between CVD categories (P= 0.008) and was more frequent in maternal congenital heart diseases; There were no differences in anatomical, infectious, and vascular pathologies between CVD categories.
Conclusions
In summary, we present a detailed evaluation of placental pathology resulting from pregnancies complicated by maternal CVD. Gross anatomic abnormalities and placental vascular pathology were more common among our cohort as a whole, and a significantly higher rate of noninfectious inflammatory conditions in the form of VUE was observed among women with CHD than among women with other forms of CVD.
Despite these findings, maternal and fetal outcomes were generally favorable. Institutional policies to routinely submit placentas for pathological examination in pregnancies complicated by maternal CVD would greatly improve our understanding of the relationship between maternal CVD and placental development. Furthermore, the study of placentas from normal and uncomplicated deliveries is needed to better understand the importance of the aforementioned findings.
Discussion
We examined placentas in a cohort of women with CVD and pathological findings correlated with cardiac disease subtypes. Gross anatomical abnormalities, inflammatory conditions, and infectious and vascular pathology were frequently observed, with 75% of placentas showing some abnormal finding.
Small placenta by weight, one of the chronic manifestations of uteroplacental insufficiency, was particularly common, as were pathological features related to poor maternal vascular perfusion. Placentas from women with CHD were significantly more likely to be affected by VUE than those from women with other forms of CVD.
Final message
- Pregnancies among women with CVD commonly show abnormal placental findings, especially anatomic and vascular pathology.
- The prevalence of vilitis of unknown etiology (VUE) differed between CVD categories. On the contrary, the incidence of specific pathological findings did not differ according to maternal characteristics.
Perspectives
Medical Knowledge : Placental development is influenced by both fetal and maternal factors during implantation, however, the influence of maternal CVD on placental health has only been studied to a limited extent. Abnormalities of placental development result in impaired uteroplacental flow and resistance and correlate with the risk of preeclampsia, fetal growth restriction, and perinatal mortality. This could be a mechanism by which maternal CVD leads to a higher rate of adverse pregnancy outcomes and may be a useful clinical indicator during routine obstetric evaluation.
Translational perspective : Our findings warrant further investigation into the relationship between maternal CVD and placental development. We believe that the presence of maternal CVD should be considered as an indication for routine submission of the placenta for detailed histopathological examination, especially given the frequency with which pathological findings were observed in our cohort of placentas.
















