Emergency Visits or Hospitalizations for Cardiovascular Diagnoses in the Post-Acute Phase of COVID-19
More than 670 million people have survived COVID-19 so far. The World Health Organization (WHO) defines long COVID as the presence of persistent symptoms more than 3 months after acute SARS-CoV-2 infection that cannot be otherwise explained and that have lasted at least 2 months. While estimates of the frequency of long COVID symptoms vary depending on the duration of follow-up, a recent systematic review of 41 studies found that 54% of COVID hospitalization survivors and 34% of non-hospitalized COVID survivors They report at least 1 persistent symptom 3 months after their infection.
However, there is debate over which of the more than 50 symptoms described by long COVID patients are actually related to their prior infection and which are simply commonly experienced by people of that age/sex, regardless of whether or not they had prior SARS-CoV. .
While a recent analysis of US claims data reported that 15% of adults younger than 65 years and 32% of those older than 65 years infected with SARS-CoV-2 developed clinical sequelae diagnosed by a who required medical attention more than 3 weeks after their acute infection, an analysis of the Veterans Affairs system suggested lower incidence rates (1.5% hypertension, 0.8% diabetes, 0.4% injury kidney and 0.4% heart failure).
However, it should be noted that all of these studies defined the “post-acute” phase as beginning 3 to 4 weeks after initial infection, which conflates early and late events and is inconsistent with the current WHO definition. Therefore, the question of which physician-assigned diagnoses are most common in the post-acute phase (i.e., after 3 months) of COVID-19 remains uncertain.
Therefore, we designed this study to examine the frequency of physician-assigned diagnoses in the post-acute phase of SARS-CoV-2 infection (i.e., more than 3 months after initial infection) and to determine which were associated with COVID-19. -19 cases with contemporary controls who had a negative reverse transcription-polymerase chain reaction (RT-PCR) test for SARS-CoV-2 performed in the same time period.
Background
Previous studies of the cardiovascular sequelae of COVID-19 include diagnoses made within 4 weeks, but the World Health Organization definition for “post-acute phase” is > 3 months.
Goals
The purpose of this study was to determine which cardiovascular diagnoses in the post-acute phase of COVID-19 are associated with SARS-CoV-2 infection.
Methods
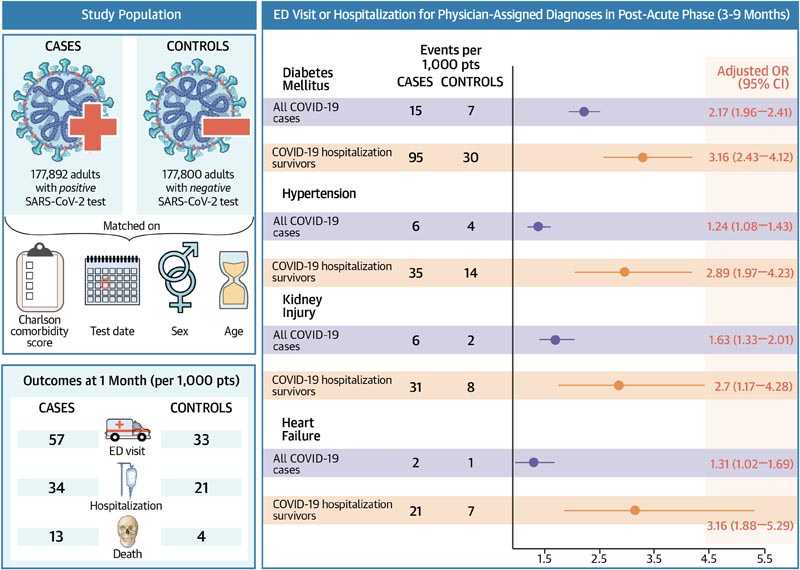
Retrospective cohort study of all adults in Alberta who tested positive for SARS-CoV-2 reverse transcription-polymerase chain reaction between March 1, 2020 and June 30, 2021, matched (by age, sex, Charlson comorbidity score, and date of testing) with controls who had a negative reverse transcription-polymerase chain reaction test.
Results
The 177,892 patients with laboratory-confirmed SARS-CoV-2 infection (mean age 42.7, 49.7% women) were more likely to visit an emergency department (5.7% vs. 3.3%), be hospitalized (3.4% vs. 2.1%) or died (1.3% vs. 0.4%) within 1 month than matched test-negative controls.
After 3 months, cases were significantly more likely than controls to have an emergency department visit or hospitalization for diabetes mellitus (1.5% vs. 0.7%), high blood pressure (0.6% vs. 0 .4%), heart failure (0.2% vs. 0.1%), or kidney injury (0.3% vs. 0.2%).
In the 6,030 patients who had survived a COVID-19 hospitalization, post-acute risks were substantially higher for diabetes mellitus (9.5% vs. 3.0%, adjusted odds ratio [aOR]: 3. 16 [95% CI: 2.43-4.12]), hypertension (3.5% vs 1.4%, aOR: 2.89 [95% CI: 1.97-4.23]), heart failure cardiac (2.1% vs. 0.7%, aOR: 3.16 [95% CI: 1.88-5.29]).
Discussion
Our study demonstrated a significant increase in emergency department visits or hospitalizations for assigned medical diagnoses of diabetes mellitus, hypertension, heart failure, or kidney injury during the post-acute phase (i.e., more than 3 months after acute infection) of COVID-19 . This finding was robust even if we restricted our analysis to only new diagnoses of each condition, and the associations were strongest in those patients who had been hospitalized for their COVID-19.
In fact, some additional associations, such as an increased risk of venous thromboembolic disease or bleeding during the post-acute phase, were only seen in COVID-19 survivors who had been hospitalized for their infection. After excluding events in the first 3 months, we found no excess risk of other commonly cited sequelae of SARS-CoV-2 infection compared to test-negative age/sex/comorbidity-matched controls, such as coronary syndrome acute, stroke or atrial fibrillation. This is important information that can help inform the debate about which reported symptoms or conditions detected in COVID-19 survivors are actually associated with prior infection and which are simply common in people of that age/sex, regardless of whether they had or not antecedents. SARS-CoV-2 infection.
Conclusions In conclusion, we have demonstrated the absolute and relative risks of cardiovascular diagnoses requiring emergency department visits or hospitalizations in the post-acute phase after SARS-CoV-2 infection, which will help inform planning for future needs. medical care and what conditions COVID-19 survivors should be screened for. However, more research is needed to examine differences between the variants of interest, particularly the Omicron variant that has been dominant since December 2021, and to determine whether vaccination (with or without booster doses) affects cardiovascular outcomes in the post-acute phase of COVID-19. Clinicians should screen COVID-19 survivors for diabetes mellitus, hypertension, heart failure, and renal dysfunction in the post-acute phase. |