Highlights
|
Background and objective
The neurological sequelae of coronavirus disease 2019 (COVID-19) may persist after recovery from an acute infection. Here, we aimed to describe the natural history of neurological manifestations more than 1 year after COVID-19.
Methods
A prospective, multicenter, longitudinal cohort study was conducted in COVID-19 survivors. At a 3-month and 1-year follow-up, patients were evaluated for neurological deficits using a neurological examination and a battery of standardized tests that included assessment of hyposmia (16-item Sniffin’ Sticks test), cognitive deficits (Cognitive Assessment of Montreal < 26) and mental health (Hospital Anxiety and Depression Scale and Post-Traumatic Stress Disorder Checklist 5).
Results
Eighty-one patients were evaluated 1 year after COVID-19, of whom 76 (94%) patients completed 3-month and 1-year follow-up.
The patients were 54 (47-64) years old and 59% were men. New and persistent neurological disorders were found in 15% (3 months) and 12% (10/81; 1 year).
Symptoms at 1-year follow-up were reported by 48/81 (59%) patients, including fatigue (38%), concentration difficulties (25%), forgetfulness (25%), sleep disorders (22%), myalgia (17 %), weakness in the extremities (17%), headache (16%), altered sensation (16%) and hyposmia (15%).
Neurological examination revealed findings in 52/81 (64%) patients with no improvement over time (3 months, 61%, p = 0.230) including objective hyposmia (Sniffin’ Sticks test <13; 51%). Cognitive deficits were evident in 18%, while signs of depression, anxiety, and post-traumatic stress disorders were found in 6%, 29%, and 10%, respectively, one year after infection.
These mental and cognitive disorders had not improved after the 3-month follow-up (all p > 0.05).
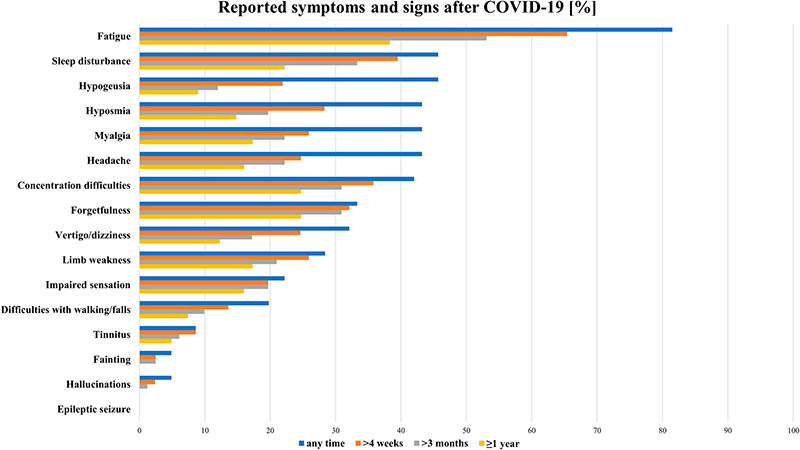
Self-reported symptoms quantified by duration (any time, >4 weeks, >3 months, ≥1 year)
Conclusion
Our data indicate that a significant number of patients still suffer from neurological sequelae, including neuropsychiatric symptoms, 1 year after COVID-19, requiring interdisciplinary management of these patients.
Discussion
In this prospective longitudinal observational study, the natural history of neurological recovery from COVID-19 up to 1 year after diagnosis is described. The focus was on new and persistent neurological symptoms and diseases, as well as measures of fatigue/mental health in a mixed outpatient and inpatient population.
New-onset, mostly mild, neurological disease was found in 12% of the cohort within 12 months of COVID-19. The most common self-reported ongoing symptom was fatigue (38%), followed by concentration difficulties (25%), forgetfulness (25%), and sleep disturbances (22%).
Objective and relevant neurological signs are described in 64% of patients, with objective hyposmia (51%) being the most prevalent symptom. Impaired cognition (18%), signs of anxiety (29%), and depression (6%) were still present in a considerable number of patients.
It is now well accepted that COVID-19 can affect human health beyond acute infection.
In addition to pulmonary manifestations and other organ dysfunctions, neuropsychiatric symptoms and signs draw attention as long-term effects of COVID-19, with common representations being fatigue, headache, and attention disorders.
















